Definition and overview of Thymoma and Thymic Carcinoma
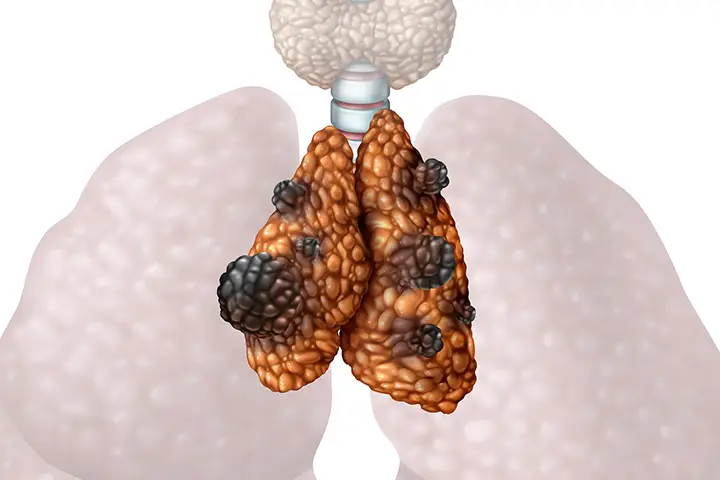
Thymoma and Thymic Carcinoma are two forms of tumors found within the thymus gland – an organ located behind the breastbone in the chest cavity that plays an essential part in immune cell production and maturation, specifically T lymphocytes or T cells.
Thymoma carcinoma:
Thymomas, or Thymic epithelial cell tumors, are rare tumors originating in the epithelium cells of the thymus that tend to grow slowly with more favorable prognoses compared to other thymic tumors. Thymomas tend to remain contained within their original location within the thymus at initial stages before potentially invading nearby structures in advanced stages.
Thymic Carcinoma:
Thymic carcinoma, another rare and aggressive cancer originating in thymus epithelial cells, tends to grow quickly, spreading out more widely throughout organs or tissues within the body, and is often diagnosed at more advanced stages than its counterpart thymoma. Both conditions typically carry poor prognoses compared to one another.
Note that though thymoma and thymic carcinoma both stem from the thymus gland, they represent two separate entities with distinct biological behaviors, treatment approaches, prognoses, and prognoses. Differentiating between them is crucial in order to provide accurate management strategies and determine an individualized course of treatment for those living with either condition.
Importance of understanding the differences between thymoma and thymic carcinoma
As it’s easy to distinguish the differences between thymoma (thymic carcinoma) and thymoma, both diseases need to be properly diagnosed in order to properly manage them.
- Accurate Diagnosis: Thymoma exhibits unique clinical and pathological traits. To accurately diagnose and plan treatment for it, it’s crucial to distinguish these two entities based on clinical presentation and pathological examination alone. Misdiagnosing either may result in delays to therapy and potentially ineffective remedies being utilized.
- Treatment Selection: Thymoma treatment differs significantly from that of thymic cancer; typically surgical resection with adjuvant treatments like chemotherapy or radiation therapy depending on its stage, with adjuvant therapies like chemotherapy or radiation therapy as needed for adjuvant therapy depending on its stage. Thymic cancer tends to be more aggressive, thus necessitating more intensive plans including surgery, radiotherapy, chemotherapy immunotherapy targeted therapy or targeted therapy as needed; understanding your specific tumor before choosing appropriate remedies is also key! When selectinging effective therapies!
- Prognostic Significance: Thymoma and thymic cancer each present unique prognostic outcomes for their respective patients. Thymoma typically offers long-term survival when detected early; on the other hand, aggressive metastases from thymic carcinoma worsen its outlook significantly. By distinguishing between them healthcare professionals can offer accurate prognostic data to their patients so they may make informed choices and plan for their future accordingly.
- Research and Clinical Trials: It is crucial that researchers understand the difference between thymic cancer (thymoma) and thymoma for effective studies on genetics, mechanisms and treatment options specific to each tumor type. Knowing their distinction will assist clinical trials investigating new therapies or targeted treatments with proper patient selection as well as evaluation of treatment outcome evaluation.
Understanding the differences between thymoma, thymic cancer, and their prognostic assessments is integral for accurate diagnosis, treatment selection, research advancement and appropriate treatments for each rare tumor type. Healthcare providers need this knowledge in order to optimize patient care and achieve improved results while contributing to new therapeutic solutions more effective against rare tumors.
Comparison table of Thymoma and Thymic Carcinoma
Certainly! This table highlights the key differences between thymoma (thymic cancer) and thymoma:
| Aspect | Thymoma | Thymic Carcinoma |
|---|---|---|
| Origin | The thymus epithelial cell line is the source of this tumour. | The thymus epithelial cell line is the source of this cancer. |
| Growth Pattern | Slow-growing crops are typical | Rapidly growing and often aggressive |
| Metastasis | The thymus is the most likely place where it tends to be localized | Metastasis to other organs is more likely |
| Prognosis | Prognosis is generally favorable | It is often associated with a worse prognosis |
| Treatment Approach | The primary treatment is surgical resection | Requires more comprehensive treatment including surgery, radiation, chemotherapy, targeted therapy or immunotherapy |
| Staging and Grading | There are many different staging and grading system available | There are many different staging and grading system available |
| Syndromes Associated with Associated Syndromes | Can be associated with paraneoplastic or autoimmune syndromes | Can be associated with paraneoplastic syndromes |
| Age at Onset | Peak incidence occurs in the 4th through 6th decade of life | Peak incidence occurs in the 6th and 7th decade of life |
Follow-up and Surveillance
After treatment for thymoma or thymic cancer, it’s crucial that patients monitor their health to detect potential recurrences, manage side effects and provide supportive care. The frequency and extent of follow-up will depend on factors like disease stage/treatment regimen as well as overall patient health status.
Here are a few considerations when planning surveillance/follow-up:
Regular Monitoring:
- Annual physical exams should be scheduled in order to maintain your general wellbeing and check for any new symptoms that arise.
- Imaging studies such as chest X rays, computed-tomography (CT), or magnetic resonance imaging may be performed to monitor any possible recurrences or metastasis of cancer in the chest area.
- Blood tests to detect tumor markers or organ function as required are conducted as necessary.
Recurrence Detection:
- Recurrence Detection Recognize and understand the telltale symptoms and signs that suggest recurrence; for instance persistent coughing, chest pains, breathing difficulty or sudden weight loss could all indicate it’s time to seek medical help again.
- Report any symptoms which cause concern to your healthcare provider as soon as possible.
- Imaging results should be carefully observed to detect signs of cancer metastasis or recurrence.
Long-Term Treatment Plan (LTTP):
- This strategy involves managing any potential side effects associated with treatment such as respiratory or cardiovascular ailments as well as any hormonal conditions or disorders that arise afterward.
- Referral to specialists such as cardiologists or pulmonologists for tailored treatment is also possible.
- As cancer can be difficult, and its treatments even more so, supporting mental and emotional well-being of cancer patients and survivors is of vital importance.
Health Lifestyle Promotion efforts:
- Encourage a healthy lifestyle including regular physical exercise and eating nutritious food to lower risk for complications and promote overall wellness.
- Information and resources related to support groups, survivorship programs and counseling available for cancer patients who wish to manage long-term side effects more easily are also provided here.
- Patients must attend regular follow-up appointments as directed by their healthcare team, beginning with more frequent initial follow-ups that gradually taper off as your health improves and stabilizes. Each follow-up schedule should be customized based on patient needs and recommendations by healthcare providers.
Conclusion
Thymoma and Thymic Carcinoma are rare and complex diseases that arise in the thymus. While thymoma is often benign and slow-growing, thymic carcinoma is aggressive and requires immediate attention. Early detection, accurate diagnosis, and personalized treatment plans play a crucial role in improving patient outcomes. With ongoing research and advancements in medical science, the future holds promise for better understanding and management of these conditions.