Introduction to Myasthenia Gravis and Lambert Eaton Syndrome
Myasthenia Gravis and Lambert Eaton Syndrome (LES) are two autoimmune neuromuscular conditions with similar characteristics and mechanisms, both leading to muscle weakness. But each disease possesses unique symptoms and causes. Myasthenia Gravis (MG) is an autoimmune condition primarily affecting the neuromuscular junction – where nerves communicate with muscles – whereby antibodies produced by our immune systems mistakenly target and attack specific receptors known as Acetylcholine Receptors (AChRs), leading to reduced numbers.
The functionality of AChRs on muscle sides of neuromuscular junction, disrupting transmission between nerves and muscles and leading to muscle weakness and fatigue that worsen with physical exertion and improve with resting periods of restful rest between bouts of activity or activity and worsening/improvements with increased activity or activities, respectively.
Lambert Eaton Syndrome, also referred to as Lambert Eaton Myasthenic Syndrome (LEMS), is an uncommon autoimmune disease characterized by muscle weakness that results from dysfunction at nerve terminals rather than at neuromuscular junction itself.
LES is associated with antibodies produced to block voltage-gated calcium channels (VGCCs) at the neuromuscular junction, thus interfering with nerve signals needed to stimulate muscle contraction via chemical called acetylcholine release from nerve receptors in nerve cell bodies. People living with this condition experience muscle weakness nearer their core area that generally improves over time through repeated use.
Though both MG and LES involve immune attacks against components of the neuromuscular system, their respective causes and autoimmune responses differ substantially: in MG antibodies target acetylcholine receptors while, for LES, voltage-gated calcium channels. Diagnosing MG and LES requires a combination of clinical evaluation, electromyography (EMG) tests, blood tests to detect specific antibodies (such as anti-AChR antibodies for MG and anti-VGCC antibodies for LES) in blood samples taken, EMG studies as well as other forms of diagnostic procedure like imaging studies.
Treatment options vary for both MG and LES; in general, medications to increase acetylcholine levels or suppress immune systems, surgical removal of the thymus gland, plasmapheresis or intravenous immunoglobulin therapy (IVIG therapy). Meanwhile for LES treatment may involve medications designed to enhance neuromuscular transmission or plasma exchange as LES is typically associated with small cell lung cancer.
While MG and LES may appear to be separate conditions, they both belong to an umbrella of autoimmune neuromuscular disorders; therefore accurate diagnosis and management are key in optimizing quality-of-life for those affected.
Brief Overview of autoimmune neuromuscular disorders
Autoimmune Neuromuscular Disorders, often referred to simply as ANDs, Refer to Conditions wherein components of the nervous system are attacked by Immune system cells resulting in muscle weakness and Dysfunction. They arise when this protective measure mistakenly misidentifies normal neuromuscular components as dangerous substances threatening the body, rather than protecting against potential threats such as chemicals found outside.
Autoimmune neuromuscular diseases occur when antibodies produced by our immune systems target specific proteins or receptors involved in communicating between muscles and nerves, disrupting normal signal transmission between them and leading to muscle fatigue and weakness due to interrupted communication pathways between muscle groups and nerves. Such disorders may affect nerves, neuromuscular junctions, or muscles themselves directly.
Autoimmune neuromuscular diseases include Myasthenia Gravis, Lambert Eaton Syndrome, and various myopathies such as polymyositis or dermatomyositis – each having different clinical presentations but all sharing one element – an immune system dysfunction leading to muscle weakness. Uncertain causes for autoimmune Neuromuscular Diseases remain, though genetic and environmental triggers, as well as abnormalities of the immune system, are all believed to play a part. Diagnosing such illnesses typically involves clinical evaluation combined with electromyography tests (EMG), blood tests to detect antibodies and imaging studies.
Autoimmune neuromuscular diseases currently do not have a cure, yet. There are, multiple treatment options to manage symptoms and slow disease progression; medications to inhibit immune reactions; plasmapheresis to remove harmful antibodies from blood); intravenous Immunoglobulin Therapy (IVIG); as well as physical therapy treatments can all help manage symptoms while slowing the disease’s progress.
Myasthenia Gravis (MG)
Myasthenia Gravis (MG) is an autoimmune condition primarily affecting the neuromuscular junction, where nerves connect with muscles. MG manifests with muscle weakness and fatigue that worsens with activity but improves with rest.
In multiple sclerosis (MG), the immune system accidentally produces antibodies which mistakenly attack specific receptors called Acetylcholine Receptors (AChRs) on muscle side of neuromuscular junction. AChRs play an integral part of transmitting nerve signals into muscles by binding with Acetylcholine as chemical messenger, so interference by antibodies disrupting them leads to muscle weakness and ultimately leads to neuropathy.

It remains difficult to ascertain the precise cause of MG. Researchers believe its development involves both genetic and environmental elements. Immune system dysfunction could play a part. Autoantibodies production could also play an integral role.
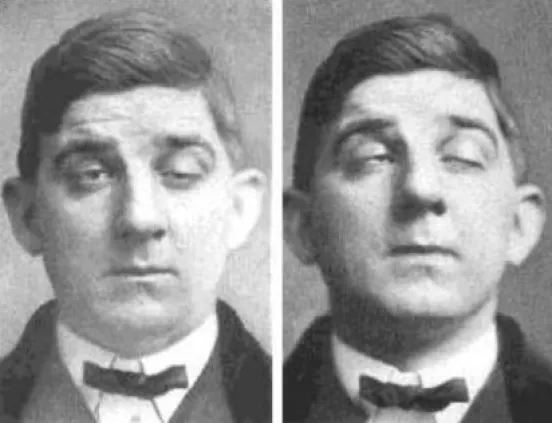
Muscle weakness (MG) is one of the key symptoms associated with myasthenia gravis (MG), commonly impacting muscles that control eye movement, facial expressions, chewing, swallowing and breathing. The weakness may become more pronounced after periods of activity; other symptoms could include drooping eyelids (ptosis), double vision (diplopia), difficulty speaking clearly as well as weakness in various body areas and in particular legs.
Diagnosing MG requires both clinical assessment and specific tests. After Conducting a Comprehensive physical exam that Assesses muscle strength and fatigue levels, Electromyography (EMG), which measures electrical activity within muscles, may also be performed to evaluate Neuromuscular Function. Blood tests may also be ordered to detect specific antibodies such as anti-AChR or anti-MuSK antibodies in blood samples; imaging studies such as chest CT scan may be recommended to check for anomalies within the thymus gland – something often associated with MG diagnosis.
Treatment options for MG aim to alleviate symptoms and restore muscle function, via medication such as cholinesterase inhibitors that increase the amount of acetylcholine available at neuromuscular junction. Immunosuppressive agents like corticosteroids may be prescribed in order to suppress immunity; surgery such as thymectomy may be advised in more severe cases.
Plasmapheresis provides harmful antibodies are removed from blood by drawing plasma out, while intravenous immunoglobulin therapy uses immune system proteins from immune system proteins which modulates immune responses in an effort to ease symptoms and modulate immune responses.
Individuals living with MG may benefit from careful management to see significant relief of symptoms and an overall increase in quality of life. Following up regularly with healthcare professionals may help detect changes or flare-ups of symptoms; any needed adjustments should be addressed quickly as necessary to keep progress going smoothly.
Lambert Eaton Syndrome (LES)
Lambert Eaton Syndrome (LES), more commonly referred to as Lambert Eaton Myasthenic Syndrome (LEMS), is an uncommon autoimmune disease characterized by muscle weakness that originates with dysfunction at nerve terminals rather than at neuromuscular junctions themselves.
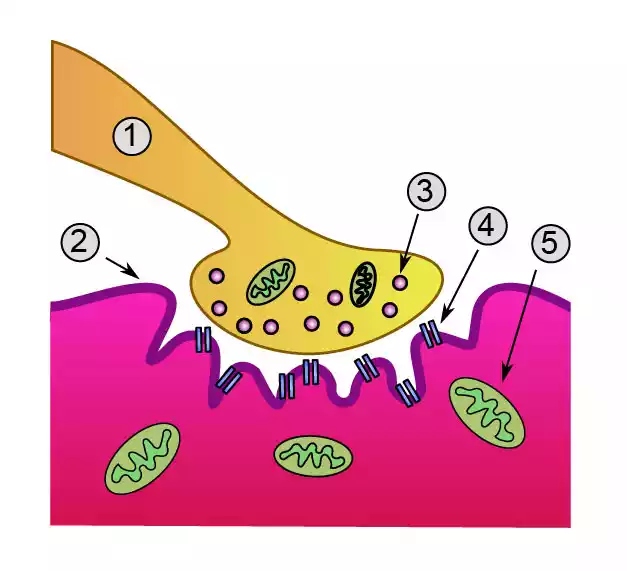 At LES, the immune system produces antibodies that target voltage-gated calcium channels (VGCCs) located on the nerve side of the neuromuscular junction. These antibodies hinder proper functioning of these VGCCs which regulate release of an important chemical called acetylcholine; which stimulates muscle contraction when released through nerve signals.
At LES, the immune system produces antibodies that target voltage-gated calcium channels (VGCCs) located on the nerve side of the neuromuscular junction. These antibodies hinder proper functioning of these VGCCs which regulate release of an important chemical called acetylcholine; which stimulates muscle contraction when released through nerve signals.
An impaired release of acetylcholine causes muscle weakness in proximal muscles nearer to the center of your body, known as “proximal muscles.” Over time this weakness often improves with use; known as the “warm-up phenomenon.” Unlike Myasthenia Gravis (MG) which worsens over activity levels; individuals living with LES often see strength increase with continued muscle use.
Less severe forms of LES have often been linked with small-cell lung cancer (SCLC), due to tumor cells secreting proteins that stimulate immune system antibodies targeting VGCC not everyone with LES also has associated cancerous growths.
Diagnosing LES involves both clinical evaluation and specific diagnostic tests. Electromyography (EMG) can be used to assess nerve and muscle function; blood tests can detect specific antibodies such as anti-VGCC antibodies; additional imaging studies may also be undertaken in order to detect and assess any possible malignancies that might exist beneath its surface.
Treatment options for LES typically involve managing symptoms while simultaneously treating its root cause if present. Medication to enhance neuromuscular transmission such as 3,4-aminopyridine (3,4-DAP) may help strengthen and function of muscles more effectively while cancer treatments could bring relief in their symptoms; other supportive measures including physical therapy or occupational therapy could also aid.
The prognosis for LES depends upon its cause and how an individual responds to treatment, but early diagnosis and appropriate management can significantly enhance quality of life for those affected by it – especially when cancer treatment has been successful. Regular visits with healthcare professionals should help monitor symptoms, adjust treatment strategies as necessary and identify complications or recurrences early.
Differences between Myasthenia Gravis and Lambert Eaton Syndrome
Myasthenia Gravis (MG) and Lambert Eaton Syndrome (LES) can differ significantly in many respects, including underlying mechanisms, neuromuscular junction involvement, symptoms distribution patterns, antibody involvement responses to treatment as well as their frequency/prevalence rates.
Let’s investigate their differences:
1. Underlying Mechanisms:
- MG: Autoantibodies target and attack acetylcholine receptors (AChRs) on muscle side of neuromuscular junction and inhibit signal transmission.
- LES: Autoantibodies targeting voltage-gated calcium channels (VGCCs) on the nerve side of neuromuscular junction can decrease release of acetylcholine.
2. Neuromuscular Junction Involvement:
- MG: Neuromuscular junction dysfunction affects nerve signals from nerve terminals directly rather than at the neuromuscular junction itself.
- LES: Dysfunction occurs at the nerve terminals rather than at the neuromuscular junction itself.
3. Distribution of Symptoms:
- MG: Muscle weakness can impact various muscle groups, including those controlling eye movements, facial expressions, chewing, swallowing and breathing.
- LES: Proximal muscles closest to the core often show weakness that can also involve the arms and trunk as symptoms may present itself with muscle cramps in these locations.
4. Response to Treatment:
- MG: Responds well to treatment with cholinesterase inhibitors, immunosuppressive drugs, thymectomy, plasmapheresis and intravenous immunoglobulin therapy (IVIG).
- LES: May benefit from medications to enhance neuromuscular transmission or plasma exchange as well as management of any cancer present if present.
5. Incidence and Prevalence:
- MG: More common than LES in terms of overall prevalence.
- LES: often associated with small cell lung cancer.
Noting the similarities and variations between MG and LES disorders is essential in providing accurate diagnoses that lead to appropriate management plans for these autoimmune neuromuscular conditions. While each condition possesses some distinguishing features, both fall under autoimmune neuromuscular disorder umbrella. Professional diagnosis by healthcare practitioners will enable accurate differentiation as well as appropriate management solutions.
Similarities between Myasthenia Gravis and Lambert Eaton Syndrome
Myasthenia Gravis (MG) and Lambert Eaton Syndrome (LES), though distinct in terms of nature and impact on neuromuscular system function, do share some striking parallels that reveal some similarities in terms of impactful on neuromuscular system functioning.
Here are MG and LES similarities in more depth:
- Autoimmune Origin: Both MG and LES are autoimmune conditions wherein the immune system attacks components of the neuromuscular system mistakenly, producing antibodies targeting specific proteins involved with neuromuscular transmission.
- Neuromuscular Dysfunction: Both MG and LES lead to neuromuscular dysfunction, leading to muscle weakness. Any disruptions in nerve signals reaching muscles cause weakness and fatigue resulting in decreased ability and performance from affected muscle fibers.
- Symptom Overlap: Individuals living with both MG and LES often exhibit overlapped symptoms. Both conditions cause muscle weakness that impacts various muscle groups in daily activities like eye movement, facial expressions, swallowing and limb movements.
- Impact on quality of life: Both Muscular Dystrophy (MG) and lower extremity spasticity syndrome (LES) have the ability to significantly diminish the quality of life due to muscle weakness and associated symptoms, impacting mobility, independence, and Physical Functioning in an individual.
Even though both conditions share similarities, it is essential to recognize their distinct underlying mechanisms, antibody targets and response rates to treatment. Accurate diagnosis by healthcare professionals is vital in distinguishing between them as well as providing management strategies tailored for affected individuals.
Summary
Myasthenia Gravis and Lambert Eaton Syndrome are complex neuromuscular disorders that require comprehensive understanding and proper management. While they present distinct challenges, advancements in research and medical care offer hope for better outcomes. With early diagnosis, effective treatment, and strong support systems, individuals living with MG or LES can lead fulfilling lives.