Introduction
Deep Vein Thrombosis and Varicose Veins can often be confused. Although both conditions affect veins, each condition has distinct causes and characteristics; to ensure appropriate medical attention and treatment it’s crucial that DVT and varicose veins be distinguished as separate entities.
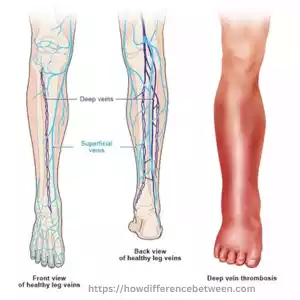
Definition of Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis (DVT) is a medical condition marked by blood clot formation within deep veins located within muscles in the legs – often leading back toward the heart and leading to complications like DVT. When blood clots form within these deep veins they cannot return blood back upstream where it belongs – to your heart! This may result in serious medical consequences including embolisms that require hospitalization to reverse and return blood back home where its required.
Once a blood clot forms in any of these veins, it can significantly obstruct or partially block blood flow causing various complications to surface. DVT should be taken very seriously because blood clots that break loose could travel through your veins to reach the lungs and potentially cause life-threatening complications known as pulmonary emboli.
Risk factors of DVT include prolonged inactivity, surgery, pregnancy, obesity and smoking as well as certain medical conditions (cancer or clotting disorders), use of hormonal contraceptives or prolonged immobility. Early diagnosis and appropriate management is vital in order to avoid complications and manage DVT effectively.
Causes of DVT
Deep Vein Thrombosis can be caused by various factors including:
- Prolonged Immobility: Long-term immobility increases your risk for deep vein thrombosis (DVT). This includes long flights, bed rest following surgery or extended periods of inactivity that prevent blood from flowing freely around your legs – slowing blood flow as a result and making blood clot formation more likely.
- Surgery and trauma: Surgeries involving lower extremities or abdominal surgery can disrupt normal blood flow.
- Medical Conditions: Physical trauma to veins also puts veins at risk of DVT formation. DVT may be caused by certain medical conditions, including cancer, heart failure and kidney disease – these being among the more likely sources.
- Hormonal Factors: Hormone fluctuations related to pregnancy or hormonal contraceptives like birth control pills or patches can increase your risk for blood clot formation and blood clot formation in general. Blood clots can even form due to hormonal influences!
- Age: Aging increases the risk of DVT due to changes in vessel structure and decreased mobility, contributing to blood clot formation in later years.
- Obesity: Weight gain and obesity can strain the circulatory system, making blood flow increasingly challenging – potentially leading to blood clots.
- Family History of DVT or Other Clotting Disorders: If there is a history of DVT in your family, or another clotting disorder that increases your risk for developing it, that increases the chances of this happening to you as well.
- Smoking: Cigarettes damage blood vessels and increase DVT risk by damaging blood clotting mechanisms and increasing DVT risk.
- Varicose Veins: Varicose veins, also known as varicosities, are characterized by impaired blood circulation and weakened vein walls that increase risk for blood clot formation in veins.
This condition increases your chances of blood clot formation resulting in blood clot formation in other places in your body as well.
Presence or absence of any one or more of these factors does not equate to DVT; those at greater risk should take precaution and remain mindful of their surroundings, seeking advice and risk assessments from healthcare providers as needed.
Symptoms and Diagnosis of DVT
DVT is associated with a number of symptoms.
- Swelling: DVT can cause swelling of the arm or leg. The swelling can be localized, for example, to a particular area such as calf, thigh or ankle. It may also feel tender to touch.
- Pain or Tenderness: DVT may cause tenderness or pain in the arm or leg. The pain can worsen while standing or walking and may feel like a muscle cramp or pulled muscle.
- Warmth and redness: The skin around the vein can feel warm and look reddish. The increased blood flow in the area is causing the redness and warmth.
- Visible Veins: In some cases the affected veins can be more visible. They can appear enlarged, engorged and have a blueish or purple color.
These Symptoms can be caused by other Conditions such as cellulitis or muscle Strains. A proper diagnosis is therefore essential. DVT is diagnosed by healthcare professionals using a variety of methods, including
- Physical Exam: The healthcare provider examines the affected area to look for swelling, tenderness and warmth. They will also check if there are any visible veins. The healthcare provider may compare the affected and unaffected limbs to see if there are any differences.
- Ultrasound: Doppler ultrasonography is an invaluable diagnostic tool that can detect blood clots. Sound waves are used to create images and assess blood flow in this non-invasive procedure.
- D-Dimer Test : D-dimer test is a type of blood test which measures the substance released by a blood clot. D-dimer levels that are elevated may indicate the presence a blood clot. This test is not conclusive and is usually used with other diagnostic methods.
- Venography: A contrast dye is injected into the vein and then X-rays are taken. It allows us to observe blood flow as well as identify any blockages caused by clots.
It is important to seek medical attention immediately if DVT is suspected. Consult a medical professional if you have symptoms that may indicate DVT.
Treatment Options for DVT
Treatment for Deep Vein Thrombosis aims to decrease risk and size of blood clots while also preventing new ones from forming. Options will depend on each person’s circumstances such as severity of their clot location as well as overall health; DVT treatment options vary accordingly.
- Anticoagulant Medications:
There was one other factor which played into our hands – an acute awareness that would otherwise remain dormant until an event transpired requiring our presence – an event like when I decided I needed my medication but decided against going for it because there weren’t any suitable pharmacies near enough (too far, and/or I just wasn’t strong enough a reason why he would make more)! So here we are now, looking back with some regret at having done nothing at all about my suffering, other peoples’s contributions being:- an increase of up to 15% respectively in regards to overall effects! (source).
DVT can be effectively treated using anticoagulant medicines – more commonly referred to as blood thinners – that prevent existing blood clots from growing larger while simultaneously decreasing risk for new ones. While anticoagulants do not dissolve existing clots directly, their natural mechanisms for dissolution will take effect and these pills may come as oral tablets or injections (low-molecular-weight heparin is one example); individual factors will determine which anticoagulant is selected as well as its duration of therapy.
- Thrombolytic Treatment: When large blood clots cause severe symptoms or there is the possibility of complications, thrombolytic medication is usually recommended as it quickly dissolves the clot and provides rapid relief. Although more powerful than anticoagulants, however, there may also be increased risks of bleeding when administered in hospital settings. It should only ever be considered in extreme situations and never as an out-patient procedure.
- Compression Stockings: Compression stockings are elastic garments worn around an affected leg that improve blood circulation by exerting pressure to drive it towards the heart, thus alleviating pooled blood and decreasing swelling. They may be combined with anticoagulant medications to alleviate symptoms more rapidly while helping avoid complications that might otherwise arise from other treatments.
- Inferior Vena Cava (IVC) Filter: An IVC filter may be beneficial in certain instances, including when anticoagulant treatment is unavailable or when there remains an increased risk of blood clot travel to the lungs despite treatment. When necessary, such filters are placed into an inferior venacava vein to carry blood from lower body areas back up towards the heart – thus helping catch blood clots before they reach lung tissue and prevent their further spread.
- Ambulation and Physical Activity: DVT treatment requires physical activity in the form of regular physical exercises to promote blood circulation and stop it pooling in veins, so DVT patients are frequently encouraged to walk regularly and engage in this form of activity.
Healthcare professionals will create an individualized treatment plan tailored specifically for you and make regular assessments on its efficacy. Be sure to set regular follow-up appointments with them, communicate regularly and stay in close communication in order to reduce complications and ensure appropriate management is in place.
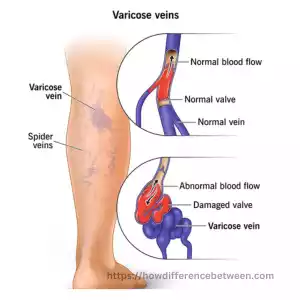
Definition of Varicose Veins
Varicose veins, commonly found near the surface of skin in legs, can become enlarged and twisty over time, typically as the walls weaken or stretch due to weakness, leading the valves within to misfunction and pool in one spot in order to flow towards heart; when these valves don’t function as they should blood pools causing further dilation of veins leading to their widening and distortion.
Varicose veins often present as bulging blue or purple veins visible through the skin, and may cause symptoms including aches, throbbing or heavy feeling in affected area, along with itchy legs or cramping sensation. Individuals suffering from varicose veins may also experience itching or cramping sensation.
Varicose veins may initially seem cosmetically aesthetic, they can often cause pain as well as serious health risks like blood clots, leg ulcers or bleeding. Factors contributing to varicose vein development include hereditary predisposition (women tend to develop them more than men), age, pregnancy obesity long duration standing or sitting and history of blood clots.
Varicose vein treatment options range from conservative measures, like lifestyle adjustments and compression stockings to more aggressive ones like sclerotherapy (injecting solutions into veins to close them off temporarily) or laser treatment based on severity, complications and individual circumstances.
Causes of Varicose Veins
Varicose veins may result from various factors, including:
- Weak or Damaged Vein Walls: Veins feature one-way valves to keep blood flowing towards the heart in its intended direction, but when these become weak or damaged they may no longer function efficiently and cause backflow of blood which pools inside veins to backflow backwards and increase varicose veins size causing them to expand and varicose further.
- Age: Varicose vein risk increases with age as veins lose elasticity and become weaker over time, becoming more vulnerable to becoming varicose veins.
- Family History of Varicose Veins: Genetic predispositions to varicose veins increase an individual’s risk, as certain individuals tend to be predisposed towards weak vein walls or broken valves that lead to varicose veins over time.
- Gender: Women have a greater risk of varicose veins due to hormonal influences related to pregnancy, menstruation cycles and menopause that contribute to their development.
- Pregnancy: While pregnant, blood volume increases to support a growing fetus and hormonal fluctuations can place additional pressure on veins leading to varicose vein development or worsening; pregnancy-induced varicose veins usually improve after giving birth and often go away within several months of giving birth on their own.
- Obesity: Carrying extra weight or obesity places undue strain on veins, making blood flow harder – leading to varicose vein formation or exacerbating existing ones. This could trigger or exacerbate existing ones.
- Prolonged Standing or Sitting: Jobs that involve prolonged standing or sitting can impair proper blood circulation and increase the risk of varicose veins, as the blood may have difficulty flowing against gravity when remaining stationary for prolonged periods.
- Lifestyle Factors: Lifestyle choices that promote varicose vein development may include physical inactivity, leading to an inactive lifestyle and crossing your legs or sitting with legs crossed regularly in such a manner that restricts blood flow.
Varicose veins increase your likelihood, but not everyone with risk factors will develop them. Maintaining a healthy lifestyle with regular exercise, elevating leg elevation and limiting extended sitting or standing times may reduce or slow the progress of varicose veins; in cases that cause discomfort or complications medical interventions like sclerotherapy, laser therapy or vein stripping may be recommended by healthcare providers as medical interventions to treat varicose veins.
Symptoms and Diagnosis of Varicose Veins
Varicose vein symptoms vary considerably among individuals; while some individuals may only experience minor discomfort, others could suffer more intensely from varicose veins.
Some of the most frequently experienced symptoms associated with varicose veins include:
- Enlarged and Bulging Veins: Varicose veins can be seen beneath the skin and appear enlarged, swollen, twisted and bulging. Their color tends toward blue-purplish hues while raising rope-like appearance is often present as well.
- Pain or Aching: People living with varicose veins frequently report experiencing discomfort in the affected areas after long periods of standing or sitting, often described as dull ache, throbbing pain or heavy legs. This pain could include dull ache, throbbing pain or heavy leg sensation.
- Leg Fatigue and Heaviness: Individuals living with varicose veins may experience feelings of leg fatigue or heaviness at the end of a day’s activity or after prolonged standing or walking sessions, especially toward evening.
- Swelling: Edema can occur in both lower legs and ankles. Overtime, swelling worsens until rest or elevation relieves it.Some individuals may experience itching or skin irritation around their affected veins.
- Skin Discoloration: Prolonged presence of varicose veins may result in skin discoloration or darkening in the lower leg area, usually within three months or less of development. Discolored areas could appear brownish-reddish in hue and feel dry or itchy;
- Complications: Varicose veins can lead to complications that include venous ulcers or bleeding. Vein ulcers develop due to inadequate blood flow and oxygen supply to the skin.
Diagnosing varicose veins typically involves being evaluated by a healthcare professional specializing in vein disorders. An examination might include:
- Visual Inspection: Healthcare providers will visually examine both legs while the person is standing or sitting to evaluate any vein-related conditions and any related symptoms.
- Medical History: Your healthcare provider will gather relevant details regarding symptoms you are experiencing, your family history of varicose veins and any previous treatments or interventions for vein related issues.
- Doppler Ultrasound: Doppler ultrasound is a noninvasive imaging technique that uses sound waves to produce images of veins and assess blood flow, creating images to pinpoint varicose veins or identify similar symptoms caused by another condition. Doppler ultrasound provides accurate identification, size and severity data on varicose veins while potentially ruling out potential alternatives that cause similar issues.
Under certain conditions, additional diagnostic tests, like duplex ultrasound or venography may be performed to provide more extensive examination of veins and blood flow.
Consultations with healthcare providers is vital in order to obtain an accurate diagnosis and appropriate management of varicose veins, with treatment plans depending on severity of symptoms, any associated risks and individual circumstances.
Treatment Options for Varicose Veins
Treatment options for varicose veins aim to relieve symptoms, improve appearance and avoid complications. Each case depends on severity of symptoms experienced as well as location/size/type/preference preferences – commonly available varicose vein treatment options include.
Lifestyle Modifications for Vein Health:
- Regular exercise: Regular Exercise, such as walking and swimming can help improve circulation and strengthen leg muscles. Its Weight management can ease pressure off veins while helping relieve symptoms.
- Leg Elevation: Elevating legs above heart level multiple times daily may help decrease swelling and improve blood flow to improve circulation and reduce swelling.
- Compression Therapy: Wearing compression stockings applies gentle pressure to the legs, helping improve blood flow and relieve symptoms. Compression stockings come in various strengths and lengths and should always be properly fitted.
- Sclerotherapy: Sclerotherapy involves injecting a solution directly into varicose or spider veins to irritate their walls, leading them to collapse and join together, eventually dissipating into your body over time. Sclerotherapy is commonly used on smaller varicose and spider veins.
- Endovenous Laser Ablation (EVLA) or Radiofrequency Ablation (RFA): Laser or radiofrequency energy are employed during these minimally invasive procedures to heat and seal off affected veins under local anesthesia; over time the vein will eventually absorb into your body naturally. Both EVLA and RFA treatments have proven their efficacy when dealing with larger varicose veins.
- Vein Stripping and Ligation: Under this procedure, an affected vein is tied off (ligated) and removed through small incisions by means of stripping (stripping). Usually used when dealing with severe cases of varicose veins.
- Endoscopic Vein Surgery: This form of vein surgery is ideal for advanced cases in which varicose veins have led to skin ulceration, using a small camera (endoscope) to view and extract them through small incisions.
As with any medical condition, vein disorders require expert assessment in order to choose an effective course of treatment for individual circumstances. Sometimes combination treatments may be recommended in order to achieve relief of symptoms, improve appearance or address complications such as venous ulcers. Regular follow up visits and ongoing monitoring is key to ensure treatment effectiveness while also addressing potential concerns that arise during therapy.
Comparison Table of Deep Vein Thrombosis and Varicose Veins
Here is a chart that highlights the differences between Deep Vein Thrombosis and Varicose Veins:
| Aspect | Deep Vein Thrombosis (DVT) | Varicose Veins |
|---|---|---|
| Definition | Formation of a blood clot deep veins | The superficial veins are enlarged, swollen and twisted |
| Cause | Blood Clot Formation | Valve walls and veins with damaged or weakened valves |
| Location | Deep veins usually found in the legs | The superficial veins are closer to the surface of the skin |
| Symptoms | Leg pain, swelling, warmth, redness, cord-like appearance | Enlarged, twisted veins, leg pain, swelling, itching, skin discoloration |
| Severity | It can cause pulmonary embolism or chronic venous failure. | It is not usually life-threatening but it can cause discomfort or cosmetic concerns. |
| Complications | Chronic venous insufficiency, pulmonary embolism | Venous ulcers, bleeding due to ruptured veins |
| Treatment | Anticoagulant medication, thrombolytic treatment, IVC filter | Surgery, sclerotherapy and compression therapy are all options. |
| Life-threatening risk | Yes, | No, |
Summary and Conclusion
Deep Vein Thrombosis (DVT) and Varicose Veins (VVs) are two separate conditions affecting leg veins; each condition presents with its own set of symptoms, causes, and treatment approaches.
Deep Vein Thrombosis (DVT) refers to blood clot formation within deep veins which block circulation. If left untreated, DVT could result in complications like pulmonary embolism which require medical intervention to cure. DVT may result from factors like immobility, vein injury or medical conditions which increase risk. Early diagnosis and treatment with anticoagulant medication is key for reducing future clot formation as well as its complications.
Varicose Veins (pronounced VAY-co-see VINAYs), are enlarged, swollen, twisted veins nearer to the skin’s surface that become distended over time due to weakened or damaged valves and vein walls, often leading to discomfort, pain, cosmetic concerns or worse yet medical procedures being necessary for their removal. Treatment options available to treat varicose veins may include lifestyle modifications, compression therapy sclerotherapy endovenous ablation surgical procedures as possible options.