As two conditions that impact the quality of life and health of individuals suffering from blood-borne bleeding disorders, Thrombocytopenia and Hemophilia can both have serious ramifications on an individual. Both disorders influence how blood clots but differ significantly based on causes, symptoms and treatment options. This article seeks to provide readers with the fullest possible knowledge and understanding about both conditions while helping readers distinguish them one from another.
Thrombocytopenia
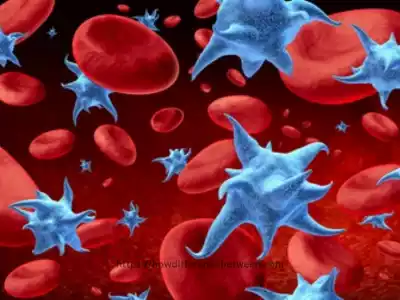
Thrombocytopenia is a condition Where a person is suffering from an abnormally low level of platelets within their Blood. Platelets are vital to clotting blood, and a decline in their number could cause excessive bleeding or bruises. This Composition focuses on the causes of Thrombocytopenia, The Symptoms, and the options for Treating Thrombocytopenia.
Causes of Thrombocytopenia
Thrombocytopenia can be caused by many factors, such as:
- Abrupt destruction by the immune system: The immune system of the body mistakenly targets and destroys Platelets.
- Bone bone marrow diseases Conditions such as leukemia or myelodysplastic syndrome may affect the production of platelets.
- Certain drugs Certain medications such as antibiotics or chemotherapy drugs, could cause a reduction in platelet count.
- Infections Infections caused by bacterial or viral infections can impact platelet production or cause their destruction to increase.
- Genetic conditions: Hereditary conditions such as Wiskott-Aldrich syndrome and May-Hegglin anomalies can cause thrombocytopenia.
Symptoms and Diagnosis
Signs and symptoms of Thrombocytopenia:
- Easy bruising: Patients suffering from thrombocytopenia may develop bruises after minor pressure or trauma to the face.
- Petechiae: Tiny, tiny spots of purple or red which appear on the mucous membranes of the skin. Petechiae result from tiny blood vessels under the skin.
- Extended bleeding: Patients suffering from thrombocytopenia can experience prolonged bleeding following minor injuries, cuts, as well as dental surgeries. The blood could take longer than normal to clot, resulting in constant bleeding.
- Frequent nosebleeds: Nosebleeds frequently occur on their own or after minor injuries in people suffering from thrombocytopenia. A low number of platelets can make it hard for the blood vessels inside the nose to close and stop the bleeding.
- Excessive or prolonged menstrual bleeding: Menstrual bleeding that is prolonged or excessive Women with thrombocytopenia can suffer from longer and heavier menstrual cycles than normal.
- Urine or stool blood: Thrombcytopenia can result in bleeding in both the urinary and digestive systems, producing blood in urine or stool samples.
- Fatigue and weakness: Anemia and fatigue which may occur because of continuous bleeding, can cause symptoms of weakness, fatigue and lightheadedness.
Diagnostics of Thrombocytopenia:
- Medical History and Physical Examination: A healthcare professional will carefully consider any medications, symptoms, or illnesses which might contribute to thrombocytopenia and conduct a physical exam as part of this evaluation Process. Physical examinations are done to determine the presence that indicate bleeding, bruises or an organ that is enlarged.
- Comprehensive blood count (CBC): A comprehensive blood count analysis measures the concentrations of platelets, red blood cells, and white blood cells present in your Blood. Low counts may signal increased thrombocytopenia.
- Peripheral blood smear: The peripheral blood test entails looking at a blood sample through microscope to examine the size, shape and form of blood platelets. It can aid in identifying any irregularities or identify the root reasons for thrombocytopenia.
- Bone marrow aspiration and biopsy: Bone Marrow Aspiration and Biopsy in some instances bone marrow aspiration and biopsy could be conducted to assess platelet production within the bone marrow and assess any dysfunction or production processes within that could impair function of these blood-forming tissues.
People experiencing symptoms of thrombocytopenia must seek medical assistance immediately for accurate diagnoses and effective treatments that address both its cause and severity. Treatment plans will depend on which approach best addresses both of these aspects.
Treatment Options
The primary goals are increasing platelet counts and decreasing bleeding complications while treating any potential root causes if possible.
Here are a few commonly employed therapies:
- Medications:
- Immune globulins: Intravenous immuno globulin (IVIG) or anti-D immuneglobulin could be administered to boost platelet counts in specific instances of inflammation.
- Thrombopoietin receptor agonists: These drugs, such as eltrombopag and romiplostim can increase creation of platelets within the bone marrow and boost the amount of platelets.
- Transfusion of platelets: When blood transfusions become necessary for extreme cases of thrombocytopenia or active bleeding, rapid increase of platelet counts to treat or prevent bleeding episodes can be achieved quickly via donation products such as blood. These transfusions provide needed platelets quickly.
- Adjustments to medications: If thrombocytopenia is due to certain medications, your healthcare provider might consider changing or stopping the medication when it is feasible. This is carried out under medical supervision to weigh blood clotting risk against the necessity of the medication.
- Treatment of underlying diseases: In cases where thrombocytopenia results from an illness or autoimmune disease, treating its source could help boost platelets counts. This could include specific therapies, antiviral drugs or immunomodulating drugs.
- Surgery: The surgical options are spleen removal (splenectomy) and the use of shunts to redirect the flow of blood away from areas of bleeding.
- Supportive care: It’s essential for people suffering from thrombocytopenia to follow certain measures to limit the possibility of bleeding. These include avoid activities that pose the chance of injury, keeping an excellent oral hygiene routine to stop bleeding gums, and taking the appropriate safety measures to avoid injuries or falls.
The treatment method will be adapted to the individual’s needs and a close examination of the platelet count and other symptoms is required to determine the effectiveness of treatment and make needed adjustments.
Understanding Hemophilia
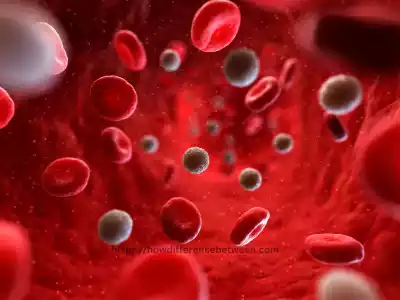
Hemophilia is a genetic disorder characterized by the inability of the blood to Clot Properly. It is primarily caused by a deficiency or absence of specific clotting factors in the blood. This section provides insights into the different types of hemophilia, their symptoms, diagnosis, and available treatment and management approaches.
Types of Hemophilia
There are two kinds of hemophilia:
- Hemophilia A The condition result from a lack of the clotting factor VIII.
- Hemophilia B also known by the name of Christmas Disease, it arises due to a deficiency in the clotting factor IX.
Symptoms and Diagnosis
Symptoms of Thrombocytopenia:
- Easy bruising: Patients suffering from thrombocytopenia might develop bruises when there is a minor injury or pressure to the face. The bruises can appear as purple or red skin discolorations.
- Petechiae: Petechiae are small, pinpoint-sized spots of red or purple which appear on the mucous membranes of the skin. Petechiae result from small, slender bleeding beneath the skin.
- Long-term bleeding: People suffering from thrombocytopenia can experience prolonged bleeding following minor injuries, cuts and dental treatments. The blood could be slower than normal to clot, resulting in continuous bleeding.
- Frequent nosebleeds: Nosebleeds frequently happen on their own or in the aftermath of minor injuries in people suffering from thrombocytopenia. The lower platelet count causes it to be challenging for the vessels within the nose to be sealed off and stop the bleeding.
- Excessive or prolonged menstrual bleeding: The menstrual cycle can be prolonged or irregular Women suffering from thrombocytopenia might suffer from longer and heavier menstrual cycles that are longer than they normally do.
- Blood in urine or stool: In the stool or urine, blood Thrombocytopenia may cause bleeding in the urinary tract as well as digestive system, resulting in blood leaking into the stool or in the urine.
- Fatigue and weakness: Anemia and fatigue that occurs due to continuous bleeding, can trigger symptoms of fatigue, weakness and lightheadedness.
Diagnosis of Thrombocytopenia:
- Physical Exam and Medical History Evaluation: A healthcare provider will carefully consider all medications, symptoms or underlying illnesses which could contribute to thrombocytopenia as they assess each patient. Physical examinations are done to determine the presence for bleeding or bruising or an organ that is enlarged.
- Comprehensive Blood Count: A comprehensive blood count test measures the amounts of platelets, red blood cells and white blood cells present in one’s blood. If one’s platelet count drops significantly then that indicates possible thrombocytopenia (low platelets count).
- Peripheral blood smear: An smear of peripheral blood is the examination of a blood sample using microscopes to determine the size, shape as well as appearance of the platelets. It can aid in identifying any irregularities or identify whether there are any other factors that cause thrombocytopenia.
- Additional laboratory tests: Other laboratory tests Based on the probable causes of thrombocytopenia blood tests could be done to determine the function of kidneys, liver functions, clotting factors, as well as the presence of autoimmune markers.
- Bone marrow aspiration and biopsy: Bone marrow aspiration, biopsy and in certain instances an aspiration of bone marrow and biopsy can be carried out to determine the amount of and functioning of platelets inside the bone marrow. This process involves the taking of a small amount of bone marrow taken from the hipbone or sternum, under local anesthesia.
- Testing for images: Ultrasonography, CT scan or MRI could be utilized in certain instances to examine organs or regions suspected to contribute to thrombocytopenia development.
Individuals experiencing symptoms of thrombocytopenia must seek medical care immediately for proper diagnosis and management, depending on its source and severity. Individual treatment will depend on its underlying cause or cause(s).
Treatment and Management
Strategies for treating and managing thrombocytopenia vary based on its cause, the severity of symptoms, and individual patient Details. The goal of treatment should be to increase platelet counts while simultaneously decreasing bleeding-related complications while controlling its root source.
Here are a few effective approaches:
- Medications:
- Corticosteroids: Prednisone-type medicines may help suppress your immune system while simultaneously decreasing platelet destruction due to immune-mediated thrombocytopenia.
- IVIG: Intravenous Immune globulin (IVIG) It can be administered to increase the number of platelets in certain immune-mediated situations.
- Thrombopoietin receptor agonists: Thrombopoietin receptor antagonists drugs such as romiplostim or eltrombopag may stimulate the production of platelets in bone marrow and increase the number of platelets.
- Platelet transfusion: Transfusion of platelets in extreme cases of thrombocytopenia or when bleeding is present Transfusions of platelets may be required to rapidly increase the number of platelets and stop or treat bleeding episodes. Platelets can be derived from blood donated products.
- Treatment of underlying diseases: When thrombocytopenia occurs due to an underlying issue like an autoimmune disease or infection Addressing and addressing the root cause of the problem can assist in boosting the number of platelets. This could involve antiviral medication and immune-suppressing drugs as well as specific treatments that target the underlying problem.
- Splenectomy: For some instances of thrombocytopenia and particularly ITP (ITP) surgery to remove the spleen (splenectomy) could be considered. The spleen plays a role with the depletion of platelets which is why removing it could aid in increasing platelet counts. This procedure is generally reserved for those who are not responding to other treatments.
- Lifestyle changes and supportive care:
- Avoiding activities that pose the highest danger of injury or trauma to limit the risk of bleeding.
- Maintaining a healthy oral hygiene routine to avoid bleeding gums and dental issues.
- Utilizing protective measures like knee pads, helmets and seat belts to avoid injuries.
- A healthy lifestyle and diet to ensure overall health as well as your blood’s health.
Monitoring of the platelet count regularly and the management of symptoms is crucial to evaluate the effectiveness of treatment and to adjust treatment plans as required.
Differences between Thrombocytopenia and Hemophilia
Hemophilia and thrombocytopenia both are distinct conditions in medicine that impact blood clotting. They differ in the underlying causes, blood components that are affected and the symptoms that are specific to.
Here are the major differences between Hemophilia and Thrombocytopenia:
- Causes:
- Thrombocytopenia: Thrombocytopenia refers to a decrease in platelet count or impairment in their functioning in blood, often as the result of immune system destruction, decreased production, or an increase in platelet Consumption. It could occur for any number of reasons and could potentially impact everyday activities from driving cars and flying planes, to using medical marijuana and eating healthfully.
- Hemophilia: Hemophilia is an inherited disorder resulting in insufficient or dysfunctional production of specific blood clotting agents, most often factors VIII (hemophilia A) or factor IX (hemophilia B). These proteins play a critical role in blood clotting processes and should therefore work normally within your system.
- Blood components affected:
- Thrombocytopenia: This disease impacts platelet production which in turn prevents excessive bleeding from happening and also forms blood clots to stop excessive bleeding.
- Hemophilia: Hemophilia affects specific blood clotting factors and can lead to insufficient or malfunction of these elements. This hinders blood’s capacity to create stable blood clots.
- Symptoms:
- Thrombocytopenia: Primary symptoms of thrombocytopenia can include bruises and petechiae prolonged bleeding from trauma or cuts, nosebleeds, heavy menstrual bleeding as well as blood in stool or urine.
- Hemophilia: A common symptom of hemophilia are prolonged or unintentional bleeding, especially in joints (resulting in swelling, pain and reduced mobility) extensive bleeding from muscles, blood loss following surgeries or injuries as well as prolonged bleeding following dental procedures.
- Treatment:
- Thrombocytopenia: Treatment of Thrombocytopenia will depend upon its cause and the Intensity of Symptoms. It can involve medicines to increase the number of platelets or combat immune-mediated destruction, or platelet transfusions for severe cases, or treating the root cause if it is it is.
- Hemophilia: Treatment of hemophilia generally requires replacing the defective or malfunctioning clotting factor with intravenous infusions. This is done on-demand which means that bleeding is a possibility or as a prophylactic treatment to avoid bleeding episodes. Clotting factor concentrates that are derived from donated blood or created synthesized are used to replace therapy.
It is vital to understand that thrombocytopenia and hemophilia are linked to increased bleeding tendencies, they each have distinct reasons and require different treatment strategies.
Causes and Mechanisms
Thrombocytopenia:
- A decrease in the production of platelets: Thrombocytopenia may result from insufficient platelet production within the bone marrow, leading to low levels of platelets present within.
- Bone marrow disorders like aplastic anemia leukemia and myelodysplastic disorder.
- Radiation therapy or chemotherapy.
- Certain medications can influence platelet production like chemotherapy drugs, anticonvulsants, or antibiotics.
- Insufficiencies in nutrition, particularly vitamins B12 as well folate.
- Increased Consumption or Destruction of Platelets: Thrombocytopenia may result from the destruction or consumption of platelets. The causes of increased destruction or consumption are:
- The body’s immune system incorrectly recognizes platelets as being foreign and destroys them. This may occur in conditions like immune thrombocytopenic ppurpura (ITP) or drug-induced thrombocytopenia.
- Infections, like bacteria or viral infections.
- Autoimmune diseases, such as systemic lupus and erythematosus (SLE) and antiphospholipid disorder.
- Certain medications, for example the heparin-induced blood clot (HIT).
Hemophilia: Hemophilia is a genetic disorder that is characterized by a lack or impairment of specific blood clotting factors, specifically factor. The fundamental mechanisms are different based on the type of hemophilia.
- Hemophilia A (Factor VIII deficiency):
- Genetic Mutation Hemophilia: A usually results from a change of the gene responsible for generating factor VIII.
- Impaired Coagulation: Cascade inability or deficiency of factor VIII affects the clotting process, in particular the pathway that is intrinsic. This causes a longer activated partial thromboplastin (aPTT) (aPTT) and a failure to make solid blood clots.
- Hemophilia B (Factor IX deficiency):
- Genetic Mutation: Hemophilia B results from mutations in the gene that produces factor IX. It is also located on the X Chromosome.
- Impaired Coagulation: Cascade absence or inefficiency of factor IX can affect the pathway that is the core of the clotting process, similar to hemophilia. This causes a longer APTT and a reduced the formation of clots.
Symptoms and Diagnosis
Thrombocytopenia Symptoms:
- Petechiae: Tiny, tiny spots of purple or red which appear on the mucous membranes.
- Prolonged bleeding: People might experience a prolonged flow of blood after minor injuries, cuts as well as dental surgeries.
- Nosebleeds frequently: They can be sudden or occur in conjunction with minor trauma.
- Frequent nosebleeds: Menstrual bleeding that is prolonged or excessive Women with thrombocytopenia can suffer from longer and heavier menstrual periods that are longer than they normally do.
- Fatigue and weakness: Anemia and fatigue that occurs due to continuous bleeding, can trigger symptoms of weakness, fatigue, and lightheadedness.
Hemophilia Signs and symptoms:
- Prolonged bleeding: Patients who suffer from hemophilia can experience prolonged bleeding following surgeries, injuries or dental procedures.
- The bleeding of muscles and joints: The process of letting blood flow into joints (hemarthrosis) may cause stiffness, pain, swelling and restricted mobility. A deep muscle bleed may cause swelling and pain.
- The easiest way to bruise: Hemophilia can result in simple bruising, even in the case of minor trauma.
- Excessive bleeding: Patients may experience a sudden or excessive bleeding with no apparent cause.
- Urine or stool blood: Hemophilia can cause bleeding within the urinary or gastrointestinal tract.
The diagnosis of Thrombocytopenia:
- Physical and medical history: Healthcare providers will perform an in-depth medical history review and physical exam in order to evaluate symptoms, detect any sign of bleeding and ascertain possible reasons behind it.
- Complete blood count (CBC): Comprehensive blood count (CBC) testing measures the number of platelets present in blood. A low count indicates thrombocytopenia.
- Peripheral blood smear: An examination of blood samples in order to examine dimensions, shapes and form of blood platelets.
- Other laboratory tests: According to the probable cause other blood tests could be performed to determine the kidney function, liver functions, the clotting process or markers of autoimmune disease.
- Bone Marrow: Aspiration and Biopsy In some instances the bone marrow could be taken to determine the amount of platelets produced and determine any anomalies.
The diagnosis of Hemophilia:
- Family history and medical background: A healthcare professional will examine the medical history of the patient as well as ask about any bleeding disorders that are a part of the family.
- Clotting factor assays: Tests in blood that determine the level and activity of specific factors that clot (factor VIII, IX) to detect the presence of abnormalities or deficiencies.
- Genetic testing: Genetic tests could be used to find specific mutations in genes that are associated with hemophilia.
- Prolonged clotting time tests: Tests for prolonged clotting time test like activated partial-thromboplastin time (aPTT) or prothrombin time (PT) could be used to determine the overall function of clotting and find out if there are any issues.
- Mixing studies: Mixing studies mixing blood samples of a patient together with plasma normal to see if there are any deficiencies in clotting factors.
Treatment Approaches
Because hemophilia and thrombocytopenia each have individual causes and mechanisms behind them, treatment options vary greatly for each condition.
This article offers an overview of available remedies:
Thrombocytopenia Treatment:
- Medications:
- Corticosteroids: These antiinflammatory drugs have the power to significantly decrease immune system activity and restrict platelet destruction related to immune-mediated thrombocytopenia.
- Intravenous immune globulin (IVIG): IVIG may be used to boost platelet counts in some immune-mediated situations.
- Thrombopoietin receptor agonists: Medications such as eltrombopag and romiplostim can increase the production of platelets in the bone marrow, and boost the number of platelets.
- Transfusion of platelets
- Transfusions may be required when suffering from severe thrombocytopenia or active bleeding occurs in order to increase platelet count and treat or stop episodes of bleeding episodes. Donated blood products provide sources for platelets.
- Treatment of the underlying condition:
- If thrombocytopenia results from an underlying issue such as an autoimmune disease or infection, treating and addressing its source may help restore platelets levels to previous levels. Such measures could include antiviral medicines and immune-suppressing treatments as well as specific therapies targeting its source disease.
- Splenectomy:
- In certain cases of thrombocytopenia, specifically ITP (ITP) surgery to remove the spleen (splenectomy) might be thought of as. The spleen plays a role in destroying platelets thus removing it could assist in increasing the number of platelets. But, this procedure is usually reserved for patients who are resistant to other treatments.
- Lifestyle modifications and supportive care:
- Avoiding activities that carry an increased chance of trauma or injury to reduce the chance of bleeding.
- Maintaining a healthy oral hygiene routine to avoid bleeding gums and dental issues.
- Utilizing protective measures like knee pads, helmets and seat belts, you can avoid injuries.
- A healthy diet and lifestyle that promotes overall health as well as blood quality.
Hemophilia Treatment:
- Therapy for replacement:
- The most important aspect of treatment for hemophilia is replacing the dysfunctional or deficient hemoglobin through intravenous injections. This is done at-will which means when bleeding occurs or as a preventative treatment to avoid bleeding episodes.
- Concentrates of the Clotting Factor made from blood donated or synthesized synthetically are utilized for replacement therapy. Concentrates of factor VIII are utilized to treat hemophilia A. the factor IX concentrates may be employed to treat hemophilia B.
- Desmopressin (DDAVP):
- Desmopressin is an artificial hormone which can trigger releases of vom Willebrand factor as well as factor VIII out of the storage locations in the body. It may be beneficial in a few cases of moderate or mild hemophilia A.
- Gene therapy:
- Gene therapy is a promising method of treating hemophilia. It involves the introduction of functional copies the genes responsible for clotting in the body’s cells to create the dysfunctional or missing clotting factors. This method aims to offer an indefinite or permanent solution for hemophilia.
- Supportive care:
- Controlling bleeding episodes using appropriate measures, for example, pressing on the site of bleeding by using ice packs or immobilizing joints.
- Physical therapy and rehabilitation resolve muscle and joint problems that result from bleeding episodes.
- Training and guidance on self-care and recognizing bleeding signs, and coping with hemophilia in your daily life.
Living with Thrombocytopenia or Hemophilia
Hemophilia or thrombocytopenia requires proactive treatments and lifestyle modifications in order to decrease bleeding episodes while supporting overall health in its sufferers.
Thrombocytopenia:
- Prevention of injuries: People living with thrombocytopenia are at increased risk of Bleeding, as such, Steps must be taken to Safeguard themselves against Injuries. This includes avoiding any activities that pose the highest chance of injury, wearing the appropriate safety gear and ensuring that you are in an environment that is safe.
- Gentle oral hygiene: A healthy oral health is crucial to stop bleeding gums and dental issues. Use a soft-bristled tooth brush floss with care, beware of using aggressive brushing techniques or dental instruments that are sharp.
- Management of medication: Check in with health professionals regularly to keep track of platelet counts and adjust the treatment if necessary.
- Understanding and managing episodes of bleeding: Be aware of the symptoms of bleeding and adopt appropriate measures to stop and manage bleeding. This includes pressing the area of bleeding and using ice packs and seeking medical attention when needed.
Hemophilia:
- Routine replacement therapy: Follow the recommended treatment program for replacement therapy, which could include infusions of concentrates of clotting factor at-a-time or as a preventative treatment to avoid bleeding episodes. Be sure to adhere to the recommended schedule and dosage outlined by your doctor.
- Monitoring and self-care: learn how to self-administer clotting factor injections if necessary and observe any indications of bleeding, joint or muscle problems. Make sure to regularly communicate with healthcare professionals to ensure proper treatment and treatment.
- Physical therapy and joint protection: Make sure you protect your joints from injury and reduce bleeding in joints. Participate in the right physical therapy exercises that strengthen muscles around joints, increase joint mobility, and treat any joint problems that may be present.
- Genetic counselling and planning for families: Hemophilia sufferers should think about genetic counseling to better understand the inheritance pattern and probability of passing the disease on to children. This will help families make informed planning decisions and also provide assistance in managing the illness in the home.
- Support for the psychological and emotional aspects: A chronic condition such as hemophilia may be difficult, so it is important to look for psychological and emotional help via support organizations, therapy or therapy to manage any mental or emotional issues.
- Emergency preparedness: Plan an emergency plan in the event of bleeding events that are severe, such as knowing how to get medical attention, having emergency contact numbers and having an inventory of clotting factor concentrates easily available.
Communicating regularly with health care providers, attending educational events and staying abreast of developments in treatments and management of hemophilia/thrombocytopenia may allow those affected by it to live full and fulfilling lives while mitigating its effect on daily activities.
Summary and Conclusion
Thrombocytopenia and Hemophilia are two significant blood disorders that affect people worldwide. Understanding the causes, symptoms, and available treatment options is crucial in managing these conditions effectively. By adopting healthy lifestyle practices, seeking support from loved ones, and staying informed about the latest advancements in medical research, individuals with thrombocytopenia and hemophilia can lead fulfilling lives.