Malignant Hyperthermia and Neuroleptic Malignant Syndrome stand out as rare but potentially life-threatening conditions. Despite their differences, they both involve a dysregulation of body temperature and muscular function. We delve into the intricacies of MH and NMS, shedding light on their causes, symptoms, and management. By understanding these conditions, we empower ourselves with knowledge that could save lives in critical situations.
What is Malignant Hyperthermia?
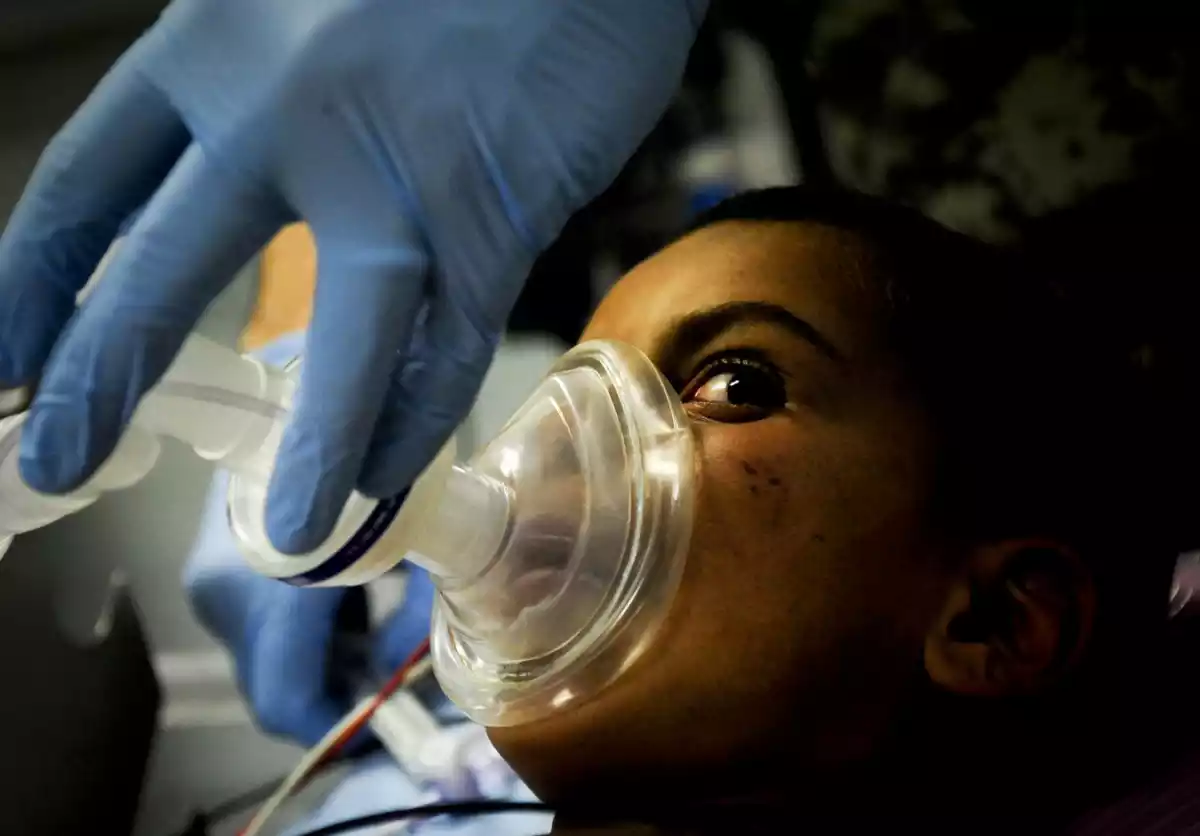
Malignant Hyperthermia (MH) is a rare but potentially life-threatening condition triggered by certain medications used during anesthesia, particularly in surgical procedures. Individuals with a genetic predisposition to MH experience an abnormal response to specific anesthetic agents. When exposed to these agents, their muscle cells undergo uncontrolled release of calcium, leading to a cascade of events that result in muscle rigidity, a rapid increase in body temperature, and metabolic acidosis.
This dangerous reaction can lead to severe complications such as muscle breakdown, organ failure, and even death if not promptly recognized and treated. Genetic mutations affecting calcium regulation in muscle cells are at the heart of MH, and immediate medical attention, along with discontinuation of triggering agents, is crucial for managing an MH crisis.
Malignant Hyperthermia is primarily characterized by its swift and often unpredictable onset. It requires a high level of vigilance from medical professionals to promptly identify and manage the condition. With advances in medical understanding and treatment strategies, the outcomes for individuals with MH have significantly improved, but the condition remains a critical concern in anesthesia and surgical settings.
Causes of Malignant Hyperthermia
Here are the causes of Malignant Hyperthermia (MH):
- Genetic Factors: MH is primarily caused by genetic mutations.
- Mutations in Muscle Genes: Mutations in genes related to calcium regulation in muscle cells are associated with MH.
- Abnormal Calcium Release: These mutations lead to abnormal calcium release within muscle cells.
- Triggering Agents: MH is often triggered by specific medications used during anesthesia, including volatile anesthetics and depolarizing muscle relaxants.
- Physical Stressors: Intense exercise, physical stress, or high environmental temperatures can also trigger MH, especially in genetically susceptible individuals.
Symptoms and Triggers
Here are the symptoms and triggers of Malignant Hyperthermia (MH):
Symptoms:
- Muscular Rigidity: Muscles become extremely stiff and rigid.
- Hyperthermia: A rapid increase in body temperature, often exceeding 104°F (40°C).
- Tachycardia: A significantly increased heart rate.
- Tachypnea: Rapid and shallow breathing.
- Metabolic Acidosis: A disturbance in the body’s acid-base balance, leading to an increase in acid levels in the blood.
- Hyperkalemia: Elevated levels of potassium in the blood, which can disrupt normal cardiac function.
- Dark Urine: Urine may become brown due to muscle breakdown.
- Altered Mental Status: Confusion, agitation, and even loss of consciousness.
- Organ Dysfunction: In severe cases, MH can lead to multiple organ failure.
Triggers:
- Anesthetic Agents: MH is commonly triggered by exposure to specific volatile anesthetics, such as halothane, sevoflurane, and desflurane.
- Muscle Relaxants: Certain muscle relaxants, particularly succinylcholine (a depolarizing muscle relaxant), can trigger MH.
- Genetic Predisposition: Genetic mutations associated with MH can make individuals susceptible to an episode when exposed to triggering agents.
- Stressful Conditions: While less common, extreme physical exertion, high environmental temperatures, and other physical stressors can trigger MH in genetically predisposed individuals.
It’s important to note that not everyone with the genetic predisposition will experience MH, but those who are at risk need to be vigilant, and healthcare providers should take precautions during anesthesia to prevent MH in susceptible patients. Immediate recognition and treatment are essential to mitigate the potentially life-threatening effects of MH.
What is Neuroleptic Malignant Syndrome?
Neuroleptic Malignant Syndrome (NMS) is a rare and serious neurological disorder that can develop as a reaction to certain antipsychotic medications, particularly those affecting dopamine receptors in the brain. The syndrome is characterized by a range of symptoms, including severe muscle rigidity, high fever, altered mental status, and autonomic dysfunction. Unlike Malignant Hyperthermia, which is triggered by anesthesia agents, NMS is triggered by medications used to manage psychiatric conditions such as schizophrenia, bipolar disorder, and other related disorders.
The exact underlying cause of NMS is not fully understood, but it is believed to result from an imbalance in dopamine signaling in the brain, particularly the disruption of dopamine transmission. This disruption can lead to dysfunction in the central nervous system’s regulation of temperature and muscle movement. NMS can progress rapidly and lead to complications such as kidney failure, respiratory distress, and even death if not promptly recognized and treated.
You might consider utilizing custom fields to organize and present information related to Neuroleptic Malignant Syndrome, such as clinical case studies, treatment approaches, and educational materials on platforms or websites focused on mental health and medical awareness.
Causes of Neuroleptic Malignant Syndrome
Here are the causes of Neuroleptic Malignant Syndrome (NMS):
- Reaction to antipsychotic medications, particularly those affecting dopamine receptors.
- Commonly associated with neuroleptic medications used to treat psychiatric disorders such as schizophrenia and bipolar disorder.
- Can occur with abrupt dosage increases or when multiple medications with similar effects are taken simultaneously.
- Disruption of dopamine signaling in the brain is believed to play a central role.
- Imbalance in dopamine levels or signaling can lead to severe muscle rigidity, hyperthermia, altered mental status, and autonomic dysfunction.
- Exact underlying mechanisms are not fully understood, but NMS is considered an idiosyncratic reaction to specific medications.
- Prompt recognition, discontinuation of triggering medications, and medical intervention are essential for managing NMS effectively.
Symptoms and Diagnosis
The symptoms and diagnosis of Neuroleptic Malignant Syndrome (NMS) are as follows:
Symptoms:
- Severe Muscle Rigidity: Profound muscle stiffness, often leading to difficulty in movement.
- Hyperthermia: Elevated body temperature, often exceeding 38°C (100.4°F).
- Altered Mental Status: Confusion, delirium, or other cognitive changes.
- Autonomic Dysfunction: Irregular blood pressure, tachycardia (rapid heart rate), diaphoresis (excessive sweating), and in some cases, fluctuations in heart rate and blood pressure.
- Tremors: Involuntary shaking or trembling of the limbs.
- Diaphoresis: Excessive sweating.
- Dysphagia: Difficulty swallowing.
- Rhabdomyolysis: An unexpected muscle fiber breakdown could potentially result in kidney damage.
- Respiratory Distress: Breathing difficulties, including rapid breathing.
Diagnosis: Diagnosing NMS involves a combination of clinical assessment, medical history, and ruling out other potential conditions with similar symptoms. Key aspects of the diagnosis include:
- Clinical Criteria: A set of established criteria that includes the presence of severe muscle rigidity, hyperthermia, and autonomic dysfunction in individuals taking antipsychotic medications.
- Exclusion of Other Conditions: The diagnosis requires ruling out other conditions that may mimic NMS, such as serotonin syndrome, malignant hyperthermia, and infections.
- Medical History: Information about recent changes in medication, dosage, or introduction of new medications, particularly antipsychotics.
- Laboratory Tests: Blood tests to assess muscle enzyme levels (indicative of muscle breakdown), electrolyte imbalances, and other metabolic changes.
It’s important to note that NMS is a medical emergency, and if suspected, immediate medical attention is crucial. Discontinuing the antipsychotic medication and providing supportive care are fundamental in managing NMS.
Comparison Table of Malignant Hyperthermia and Neuroleptic Malignant Syndrome
Here’s a comparison table highlighting the key differences between Malignant Hyperthermia (MH) and Neuroleptic Malignant Syndrome (NMS):
| Aspect | Malignant Hyperthermia (MH) | Neuroleptic Malignant Syndrome (NMS) |
|---|---|---|
| Underlying Cause | Genetic mutations affecting calcium regulation in muscle cells | Reaction to certain antipsychotic medications affecting dopamine receptors |
| Triggering Agents | Anesthesia agents, such as volatile inhalational agents and muscle relaxants | Antipsychotic medications used to treat psychiatric disorders |
| Onset of Symptoms | Rapid, often during anesthesia or surgery | Can develop gradually after starting or increasing antipsychotic medication |
| Muscle Rigidity | Present, particularly in jaw and chest muscles | Severe muscle rigidity affecting various muscle groups |
| Hyperthermia | Elevated body temperature due to increased metabolism | Elevated body temperature due to disrupted thermoregulation |
| Metabolic Acidosis | Common occurrence | Less common |
| Mental Status Changes | Typically not a prominent feature | Altered mental status, confusion, delirium |
| Dopamine Involvement | Not directly related to dopamine dysfunction | Result of disruption in dopamine signaling |
| Diagnostic Tests | Clinical signs, genetic testing, caffeine-halothane contracture test | Clinical assessment, exclusion of other conditions, medical history |
| Treatment | Discontinue triggering agents, dantrolene administration | Discontinue antipsychotic medication, supportive care |
| Complications | Rhabdomyolysis, electrolyte imbalances, organ failure | Kidney failure, respiratory distress, complications from altered metabolism |
Similarities of Malignant Hyperthermia and Neuroleptic Malignant Syndrome
While Malignant Hyperthermia (MH) and Neuroleptic Malignant Syndrome (NMS) are distinct conditions, they do share certain similarities:
- Elevated Body Temperature: Both MH and NMS are characterized by a rapid and dangerous increase in body temperature, which can have severe consequences if not promptly addressed.
- Muscle Rigidity: Both conditions involve muscle rigidity, making movement difficult and contributing to the overall clinical presentation.
- Potentially Life-Threatening: MH and NMS are both serious medical emergencies that require immediate intervention. Without proper treatment, they can lead to severe complications, including organ failure and death.
- Medication-Related: Both conditions can be triggered by medications. MH is often triggered by specific anesthetics and muscle relaxants, while NMS is associated with certain antipsychotic medications.
- Autonomic Dysfunction: Both conditions can lead to autonomic dysfunction, causing disruptions in bodily functions such as heart rate, blood pressure, and sweating.
- Complex Diagnosis: Diagnosing both MH and NMS can be challenging due to overlapping symptoms and the need to rule out other potential causes of similar clinical presentations.
- Multidisciplinary Care: Managing both conditions requires collaboration among various medical specialties, including anesthesiologists, intensivists, and critical care specialists.
- Awareness and Education: Healthcare professionals need to be aware of the signs and symptoms of both conditions to ensure prompt recognition and appropriate management.
While these similarities exist, it’s crucial to note that the underlying causes, triggers, and treatment approaches for MH and NMS are different. Therefore, accurate diagnosis and tailored management are essential for ensuring the best outcomes for individuals affected by these conditions.
Treatment Options for Malignant Hyperthermia and Neuroleptic Malign Syndrome
Treatment for Malignant Hyperthermia (MH)

Immediate action is crucial when dealing with an MH crisis. The following steps are taken to manage this life-threatening condition:
- Discontinuation of Triggering Agents: The first step is to halt the administration of the triggering anesthetic agents or muscle relaxants that initiated the MH reaction.
- Cooling Measures: Cooling the body rapidly is essential to lower the dangerously elevated temperature. Cold intravenous fluids and cooling blankets are often used for this purpose.
- Administering Dantrolene: Dantrolene, a specific medication, is the cornerstone of MH treatment. It counters the muscle contractions and helps restore normal calcium levels.
- Medical Team Collaboration: A multidisciplinary medical team, including anesthesiologists and critical care specialists, works together to provide immediate and appropriate care.
Treatment for Neuroleptic Malignant Syndrome (NMS)

Managing NMS involves the following steps:
- Discontinuation of Antipsychotic Medications: The primary action is to stop the use of the antipsychotic medication that triggered the NMS.
- Supportive Care: Providing supportive care to address symptoms is essential. This includes hydration, monitoring vital signs, and maintaining electrolyte balance.
- Medication Adjustments: Depending on the individual’s condition, alternative medications may be considered for ongoing treatment of the underlying psychiatric disorder.
- Hospitalization: Severe cases of NMS may require hospitalization for close monitoring and intensive care.
Timely intervention and close medical attention are critical to ensuring the best possible outcomes for individuals affected by these conditions. It’s important to note that management approaches may vary based on individual factors and the severity of the crisis.
Prevention and Risk Factors
Malignant Hyperthermia (MH):
- Genetic Predisposition: Individuals with a family history of MH are at higher risk. Informing healthcare providers about this history before any surgery is vital to ensure proper precautions are taken.
- Avoiding Triggering Agents: An essential preventive measure involves identifying and avoiding triggering anesthetics and muscle relaxants known to induce MH in susceptible individuals.
- Genetic Testing: Genetic testing can be performed to determine an individual’s susceptibility to MH. This can guide medical decisions and anesthetic choices.
Neuroleptic Malignant Syndrome (NMS):
- Antipsychotic Medications: The use of antipsychotic medications, particularly older typical antipsychotics, increases the risk of NMS. Healthcare providers must monitor patients closely for signs of NMS during treatment.
- Patient Factors: Certain patient factors, such as dehydration, high doses of antipsychotics, and rapid dosage increases, may elevate the risk of NMS.
Shared Preventive Measures:
- Patient Communication: Openly discussing medical history, including any previous adverse reactions to medications, is crucial to ensuring proper precautions are taken.
- Medication Review: Healthcare providers should review a patient’s current medications to identify potential interactions or contraindications.
- Individualized Care: Tailoring anesthesia and medication choices based on an individual’s medical history and risk factors is essential for preventing MH and NMS.
By understanding these risk factors and taking appropriate preventive measures, healthcare providers can minimize the occurrence and impact of these potentially life-threatening conditions.
Conclusion
Malignant Hyperthermia and Neuroleptic Malignant Syndrome emerge as distinct challenges. While sharing certain symptoms, these conditions diverge in causes, triggers, and treatment approaches.
Timely recognition, precise diagnosis, and effective intervention are paramount to ensure the well-being of individuals facing these rare yet impactful disorders. By comprehending their nuances, healthcare professionals and patients alike can navigate the path to informed decisions and improved outcomes.