Streptococcus Pneumoniae and Haemophilus Influenzae are two distinct bacterial species with significant implications for human health. Streptococcus pneumoniae, often referred to as pneumococcus, is a Gram-positive bacterium known for causing a wide range of respiratory and invasive infections, including pneumonia, meningitis, and otitis media. It is a leading cause of morbidity and mortality worldwide, particularly among vulnerable populations such as children and the elderly.
On the other hand, Haemophilus influenzae is a Gram-negative coccobacillus responsible for various infections, including influenza, meningitis, and respiratory tract illnesses. The introduction of vaccines has led to a decline in Haemophilus influenzae type b (Hib) infections, but it remains a concern in certain regions. Understanding the differences between these bacteria is crucial for effective diagnosis, treatment, and prevention strategies.
Definition of Streptococcus Pneumoniae
Streptococcus pneumoniae, often referred to simply as pneumococcus, is a bacterium belonging to the Streptococcus genus. It is a Gram-positive, facultative anaerobic coccus (spherical-shaped bacterium) that commonly inhabits the respiratory tract of humans. Streptococcus pneumoniae is a significant human pathogen known for causing a range of infectious diseases, particularly in the respiratory system.
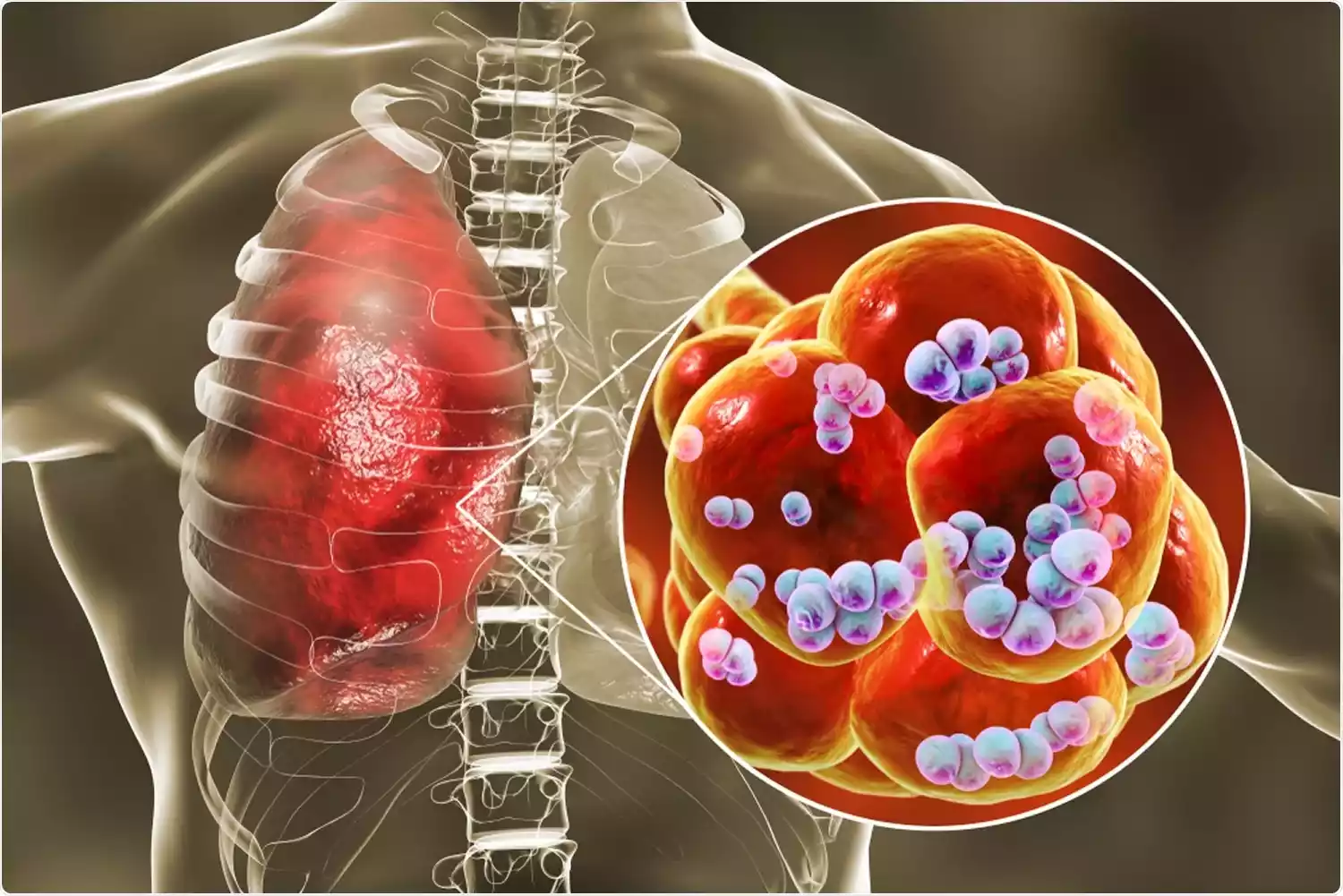
It is characterized by its polysaccharide capsule, which plays a crucial role in virulence and immune evasion. Diseases caused by S. pneumoniae include pneumonia, meningitis, otitis media, and sinusitis, among others. Understanding and effectively managing S. pneumoniae infections is essential in healthcare to prevent and treat these diseases, especially in vulnerable populations.
Definition of Haemophilus Influenzae
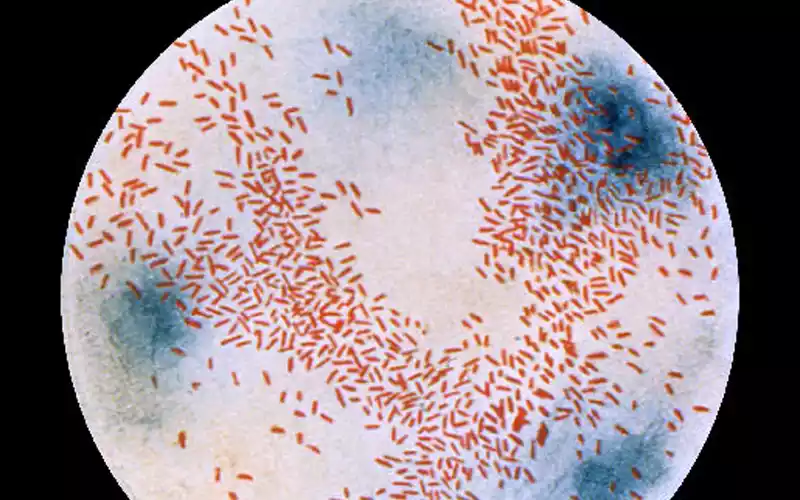
Haemophilus influenzae, often abbreviated as H. influenzae, is a Gram-negative coccobacillus bacterium belonging to the Pasteurellaceae family. This bacterium is named after its initial association with respiratory infections, even though it is not related to the influenza virus. Haemophilus influenzae is known for causing various infectious diseases in humans. It may have a polysaccharide capsule that enhances virulence, particularly in Haemophilus influenzae type b (Hib) strains.
Diseases associated with H. influenzae include invasive conditions such as meningitis, bacteremia (bloodstream infection), and pneumonia, particularly in the case of Hib infections. Non-typeable Haemophilus influenzae (NTHi) is often responsible for respiratory tract infections, including otitis media (ear infections), sinusitis, and bronchitis.
Understanding and diagnosing H. influenzae infections are essential in healthcare for appropriate treatment and preventive measures like vaccination against Hib infections, particularly in children.
Comparison table of Streptococcus Pneumoniae and Haemophilus Influenzae
Here’s a comparison table highlighting some key differences between Streptococcus pneumoniae and Haemophilus influenzae:
| Characteristic | Streptococcus pneumoniae | Haemophilus influenzae |
|---|---|---|
| Taxonomy and Classification | Gram-positive coccus | Gram-negative coccobacillus |
| Capsule Presence | Present in various serotypes | May have a capsule (Hib most notable) |
| Primary Diseases | Pneumonia, Meningitis, Otitis media, Sinusitis | Hib: Meningitis, Bacteremia, Pneumonia, NTHi: Respiratory infections (e.g., otitis media, sinusitis) |
| Transmission | Respiratory droplets | Respiratory droplets |
| Virulence Factors | Polysaccharide capsule, Pneumolysin, Autolysin, IgA1 protease | Polysaccharide capsule (Hib), Adhesins, Lipooligosaccharide (LOS) |
| Gram Staining | Gram-positive | Gram-negative |
| Cell Wall Structure | Thick peptidoglycan layer in cell wall | Thinner peptidoglycan layer, susceptible to osmotic pressure changes |
| Anaerobic/Facultative Anaerobic | Facultative anaerobe | Facultative anaerobe |
| Common Age Groups Affected | All age groups, especially elderly and children | Children, particularly infants (Hib) |
| Diagnosis Methods | Isolation from clinical samples, serotyping | Isolation from clinical samples, serotyping |
| Antibiotic Treatment | Penicillin, beta-lactam antibiotics | Ampicillin, ceftriaxone, beta-lactam antibiotics |
| Antibiotic Resistance | Increasing concern | Varied, depending on strain and resistance mechanisms |
| Vaccination | Pneumococcal vaccines available (PCV, PPSV) | Hib vaccine for Haemophilus influenzae type b |
| Preventive Measures | Public health strategies for disease control | Hib vaccination, respiratory hygiene, and infection control |
| Typical Clinical Presentation | Pneumonia, Meningitis, Otitis media, Sinusitis | Meningitis, Bacteremia, Respiratory infections |
There are multiple serotypes of both Streptococcus pneumoniae and Haemophilus influenzae, and the clinical presentation and severity of diseases may vary depending on the specific serotype involved.
Clinical Presentation
Streptococcus pneumoniae and Haemophilus influenzae can both cause various clinical presentations, primarily respiratory tract infections. Here’s a brief overview of the clinical presentations associated with each bacterium:
Streptococcus pneumoniae:
- Pneumonia: Streptococcus pneumoniae is the leading cause of bacterial pneumonia. Symptoms may include fever, cough with sputum production, chest pain, difficulty breathing, and fatigue. It can range from mild to severe, with potential complications like pleural effusion and abscess formation.
- Otitis Media: This bacterium commonly causes middle ear infections in children, resulting in symptoms like ear pain, fever, and sometimes hearing impairment.
- Sinusitis: Streptococcus pneumoniae can infect the sinuses, leading to sinusitis. These symptoms could include facial discomfort, congestion and nasal discharge.
- Meningitis: Invasive infections can lead to bacterial meningitis, a serious condition characterized by symptoms such as severe headache, fever, neck stiffness, and altered mental status. Prevalence rates are highest among young children and elderly individuals.
- Bacteremia: It can cause bloodstream infections, resulting in symptoms like high fever, chills, and general malaise.
Haemophilus influenzae:
- H. influenzae Type b (Hib): This type of Haemophilus influenzae primarily affects children and can cause various illnesses, including:
- Meningitis: Symptoms are similar to those of pneumococcal meningitis, including fever, headache, neck stiffness, and altered mental status.
- Epiglottitis: An acute and potentially life-threatening condition in children, characterized by severe sore throat, difficulty swallowing, drooling, and respiratory distress.
- Pneumonia: H. influenzae can also cause pneumonia, especially in young children.
- Non-typeable H. influenzae (NTHi): This strain is associated with a wider range of respiratory infections in both children and adults, including:
- Otitis Media: Non-typeable H. influenzae can cause ear infections with symptoms similar to those seen in Streptococcus pneumoniae infections.
- Sinusitis: Like Streptococcus pneumoniae, H. influenzae can infect the sinuses, leading to sinusitis symptoms.
The clinical presentation of these bacterial infections can vary depending on the patient’s age, overall health, and the specific strain of the bacterium involved. Additionally, vaccines have been developed to prevent some of these infections, particularly those caused by H. influenzae type b (Hib) and certain strains of Streptococcus pneumoniae, which have significantly reduced the incidence of these diseases.
Diagnosis of Streptococcus Pneumoniae and Haemophilus Influenzae
The diagnosis of Streptococcus pneumoniae and Haemophilus influenzae infections typically involves a combination of clinical evaluation, laboratory tests, and imaging studies. Here are the common methods used to diagnose these bacterial infections:
Diagnosis of Streptococcus pneumoniae Infections:
- Clinical Evaluation: The doctor will assess the patient’s medical history and perform a physical examination to look for signs and symptoms of infection, such as fever, cough, and respiratory distress.
- Chest X-ray: A chest X-ray may be performed to visualize the lungs and identify signs of pneumonia, such as lung consolidation or infiltrates.
- Sputum Culture: A sputum sample may be collected for culture to identify the presence of Streptococcus pneumoniae. Gram stain analysis on sputum can provide preliminary details about what kind of bacteria are present.
- Blood Culture: If there are signs of bacteremia or septicemia, blood cultures may be taken to detect the presence of the bacteria in the bloodstream.
- Antigen Testing: Rapid antigen tests, such as the urinary antigen test, can detect specific antigens produced by Streptococcus pneumoniae. This test is particularly useful in diagnosing pneumococcal pneumonia.
- Molecular Testing: Polymerase chain reaction (PCR) assays can be used to detect the DNA of Streptococcus pneumoniae in clinical samples.
Diagnosis of Haemophilus influenzae Infections:
- Clinical Evaluation: As with pneumococcal infections, clinical evaluation, including a medical history and physical examination, is crucial in diagnosing Haemophilus influenzae infections.
- Cerebrospinal Fluid Analysis: For suspected cases of meningitis, a lumbar puncture (spinal tap) may be performed to collect cerebrospinal fluid (CSF) for analysis. The CSF can be examined for signs of infection, such as an elevated white blood cell count, and the presence of Haemophilus influenzae can be confirmed through culture or PCR.
- Throat Swab: For respiratory tract infections or throat-related symptoms, a throat swab may be collected to identify Haemophilus influenzae through culture or PCR.
- Blood Culture: In cases of bacteremia or septicemia, blood cultures may be taken to detect the presence of Haemophilus influenzae in the bloodstream.
- Imaging: Imaging studies, such as a chest X-ray or sinus X-ray, may be performed to evaluate the extent of infection and associated complications.
- Antigen Testing: Rapid antigen tests may be available for specific Haemophilus influenzae types, such as Hib. These tests can quickly identify the presence of the bacteria in clinical samples.
The choice of diagnostic tests may vary depending on the specific clinical presentation and suspected site of infection. Early diagnosis and appropriate treatment are crucial for managing these bacterial infections effectively and preventing complications.
Treatment and Antibiotic Resistance for Streptococcus Pneumoniae and Haemophilus Influenzae
Treatment and antibiotic resistance for Streptococcus pneumoniae and Haemophilus influenzae are significant aspects of managing infections caused by these bacteria.
Streptococcus pneumoniae:
Treatment:
- Common antibiotics for treating Streptococcus pneumoniae infections include penicillins (e.g., amoxicillin), cephalosporins, and macrolides (e.g., azithromycin). The choice of antibiotic depends on the severity of the infection and local resistance patterns.
- Severe cases may require hospitalization and intravenous antibiotics, such as ceftriaxone or vancomycin.
Antibiotic Resistance:
- Resistance to antibiotics, particularly penicillin, is a growing concern for Streptococcus pneumoniae. This resistance is due to the acquisition of resistance genes.
- Multidrug-resistant strains, known as MDR pneumococci, have emerged, making treatment more challenging.
- To combat resistance, healthcare providers rely on guidelines that consider local resistance patterns when selecting antibiotics.
- Vaccination with pneumococcal conjugate vaccines (PCVs) has also helped reduce the prevalence of antibiotic-resistant strains.
Haemophilus influenzae:
Treatment:
- The primary treatment for Haemophilus influenzae infections is amoxicillin, especially for respiratory tract infections.
- For severe cases or when resistance is suspected, cephalosporins (e.g., ceftriaxone) may be used.
- Trimethoprim-sulfamethoxazole (TMP-SMX) is an alternative for certain non-typeable Haemophilus influenzae infections.
Antibiotic Resistance:
- Beta-lactamase production is a common mechanism of resistance in Haemophilus influenzae, rendering some strains resistant to amoxicillin.
- In response, doctors may prescribe alternative antibiotics or combination therapies.
- Proper vaccination with the Haemophilus influenzae type b (Hib) vaccine has significantly reduced the incidence of resistant infections.
To effectively manage these infections, healthcare providers should consider the antibiotic susceptibility of the bacteria, the patient’s clinical condition, and local resistance patterns when selecting antibiotics. Additionally, prudent antibiotic stewardship practices are crucial to mitigate the development and spread of antibiotic resistance in both Streptococcus pneumoniae and Haemophilus influenzae.
Prevention and Control
Prevention and control strategies for Streptococcus pneumoniae and Haemophilus influenzae infections primarily revolve around vaccination, antibiotic stewardship, and public health measures. Here are key aspects of prevention and control for these bacterial infections:
1. Vaccination:
- Streptococcus pneumoniae: The use of pneumococcal conjugate vaccines (PCVs) and pneumococcal polysaccharide vaccines (PPSVs) has been instrumental in preventing invasive pneumococcal disease. High vaccine coverage in children, as well as targeted vaccination of at-risk adults, is crucial to reducing disease burden.
- Haemophilus influenzae: Vaccination with the Haemophilus influenzae type b (Hib) vaccine has led to a significant decrease in Hib-related infections, especially among children. Ensuring that infants receive the recommended doses of the Hib vaccine is a primary prevention strategy.
2. Antibiotic Stewardship:
- Appropriate and judicious use of antibiotics is essential to prevent the development of antibiotic resistance in these bacteria. Healthcare providers should prescribe antibiotics only when necessary, following local guidelines and considering antibiotic resistance patterns.
3. Hygiene and Infection Control:
- Good hygiene practices, such as frequent handwashing, can help reduce the risk of respiratory tract infections caused by these bacteria. Proper respiratory hygiene, including covering one’s mouth and nose when coughing or sneezing, can also prevent the spread of respiratory droplets containing bacteria.
- In healthcare settings, infection control measures, including isolation of infected patients, proper cleaning and disinfection, and adherence to hand hygiene protocols, are essential to prevent healthcare-associated infections.
4. Surveillance and Monitoring:
- Public health agencies monitor the prevalence of Streptococcus pneumoniae and Haemophilus influenzae infections, including their antibiotic resistance patterns, to identify trends and emerging strains. This information guides vaccination programs and treatment guidelines.
5. Education and Awareness:
- Public education campaigns can raise awareness about the importance of vaccination, proper antibiotic use, and good hygiene practices to prevent infections. Healthcare providers play a crucial role in educating patients about vaccines and infection prevention.
6. Research and Vaccine Development:
- Continued research into the epidemiology and genetics of these bacteria, as well as vaccine development efforts, can lead to more effective prevention and control strategies.
7. Timely Diagnosis and Treatment:
- Early diagnosis and prompt treatment of infections are critical to preventing complications and reducing the spread of these bacteria. Healthcare providers should be vigilant in identifying and managing infections.
Preventing and controlling Streptococcus pneumoniae and Haemophilus influenzae infections require a multifaceted approach that includes vaccination, responsible antibiotic use, hygiene practices, and ongoing surveillance. Public health efforts, along with individual and healthcare provider actions, play a vital role in reducing the impact of these bacterial pathogens on public health.
Summary
Streptococcus pneumoniae and Haemophilus influenzae are two bacterial pathogens known for causing a range of respiratory tract infections and invasive diseases. Their clinical presentations, treatment options, and prevention strategies largely depend on factors such as the specific strain, patient age, and vaccination status.
Vaccination programs, proper antibiotic use, and infection control measures are vital in reducing the burden of these infections and minimizing antibiotic resistance. Continued research, surveillance, and public education efforts remain crucial in our ongoing battle against these pathogens, with the goal of improving public health and preventing the severe consequences of these infections.