Intestinal and Diffuse Gastric Cancer are two distinct subtypes of stomach cancer, each characterized by unique pathological features and clinical behaviors. Intestinal gastric cancer typically exhibits well-defined tumor structures and is often associated with pre-malignant changes in the stomach lining. In contrast, diffuse gastric cancer is characterized by the infiltration of cancer cells throughout the stomach wall, often presenting with a signet ring cell appearance.
Understanding these differences is crucial for accurate diagnosis and tailored treatment strategies to improve patient outcomes. This content outline will explore the etiology, pathological features, clinical presentation, diagnosis, treatment approaches, prognosis, and future directions for these two gastric cancer subtypes.
What is Intestinal Cancer?
Intestinal cancer is a term often used to describe a specific subtype of gastric (stomach) cancer rather than a distinct cancer type on its own. Intestinal gastric cancer refers to a type of stomach cancer that typically displays well-defined tumor structures and is associated with the presence of intestinal metaplasia, a pre-malignant change in the stomach lining where normal stomach cells transform into cells resembling those found in the intestine.
This subtype is characterized by a specific histological appearance and growth pattern, which differentiates it from other forms of stomach cancer, such as diffuse gastric cancer. Understanding these distinctions is essential for diagnosing and treating intestinal gastric cancer effectively.
Causes of Intestinal Cancer
Intestinal cancer, specifically referring to intestinal gastric cancer, is primarily associated with the stomach rather than the intestines. This subtype of gastric cancer is linked to various causes and risk factors, including:
-
- Helicobacter pylori Infection: Chronic infection with the bacterium Helicobacter pylori (H. pylori) is a significant risk factor for intestinal gastric cancer. H. pylori can lead to inflammation and damage to the stomach lining over time, increasing the risk of cancer development.
- Dietary Factors: Diets high in salt, smoked and pickled foods, and low in fruits and vegetables are associated with an increased risk of gastric cancer, including the intestinal subtype.
- Tobacco and Alcohol Use: Smoking and excessive alcohol consumption have been linked to a higher risk of gastric cancer, including the intestinal type.
- Family History: A family history of gastric cancer can increase an individual’s risk, especially if a close relative (such as a parent or sibling) has had the disease.
- Genetic Factors: Certain genetic factors and inherited conditions, such as Hereditary Diffuse Gastric Cancer (HDGC) syndrome and mutations in genes like CDH1, can predispose individuals to intestinal gastric cancer.
- Age and Gender: Gastric cancer, including the intestinal type, is more common in older individuals and tends to affect men more than women.
- Previous Stomach Surgery: Individuals who have had partial gastrectomy (removal of a portion of the stomach) for other reasons may have an increased risk of gastric cancer.
- Geographic Location: The incidence of gastric cancer varies by geographic region, with higher rates reported in some parts of Asia, South America, and Eastern Europe.
- Occupational Exposures: Some occupational exposures, such as working in coal mines, have been associated with an increased risk of gastric cancer.
While these factors are associated with an increased risk of intestinal gastric cancer, not everyone exposed to these risk factors will develop the disease. Additionally, early detection through regular medical check-ups and screenings can improve outcomes, as gastric cancer, when diagnosed at an early stage, is often more treatable. If you have concerns about your risk of intestinal gastric cancer or other gastrointestinal conditions, it’s advisable to consult with a healthcare professional who can provide personalized guidance and recommendations.
Symptoms of Intestinal Cancer
Intestinal gastric cancer, which is a subtype of stomach cancer, can manifest with various symptoms. However, it’s important to note that the symptoms of intestinal gastric cancer can be similar to those of other gastrointestinal conditions, making early diagnosis challenging. If you experience persistent or concerning symptoms, it’s crucial to seek medical evaluation.
Common symptoms of intestinal gastric cancer may include:
-
- Indigestion: Persistent or recurrent indigestion or dyspepsia, characterized by discomfort or burning sensations in the upper abdomen.
- Abdominal Pain: Chronic or intermittent abdominal pain or discomfort, which may be vague or localized in the upper abdomen.
- Nausea and Vomiting: Frequent nausea, sometimes accompanied by vomiting, especially after eating.
- Unexplained Weight Loss: Significant and unexplained weight loss, often associated with a decreased appetite.
- Loss of Appetite: A noticeable reduction in appetite, leading to decreased food intake.
- Early Satiety: Feeling full quickly or after consuming small amounts of food, which can contribute to unintentional weight loss.
- Fatigue: Ongoing fatigue or weakness, which may result from anemia due to bleeding from the stomach lining.
- Blood in Stool or Vomit: Occasional or recurrent bleeding from the stomach may lead to the presence of blood in stools (melena) or vomiting of blood (hematemesis).
- Difficulty Swallowing: Dysphagia, or difficulty swallowing, can occur when the tumor grows and obstructs the passage from the stomach to the small intestine.
- Persistent Heartburn: Chronic heartburn, also known as gastroesophageal reflux disease (GERD), can be associated with intestinal gastric cancer.
- Paleness: Anemia-related symptoms, such as paleness of the skin and fatigue, can develop if the cancer causes chronic bleeding.
- Swollen Lymph Nodes: Enlarged lymph nodes in the neck, armpits, or groin may indicate advanced stages of the disease.
It’s essential to recognize that these symptoms can vary in severity, and some individuals may experience only a few of them. Furthermore, many of these symptoms are non-specific and can be caused by various gastrointestinal conditions. Therefore, a thorough medical evaluation, including physical examinations, endoscopic procedures (such as gastroscopy), imaging tests, and biopsies, is necessary to diagnose intestinal gastric cancer accurately.
What is Diffuse Gastric Cancer?
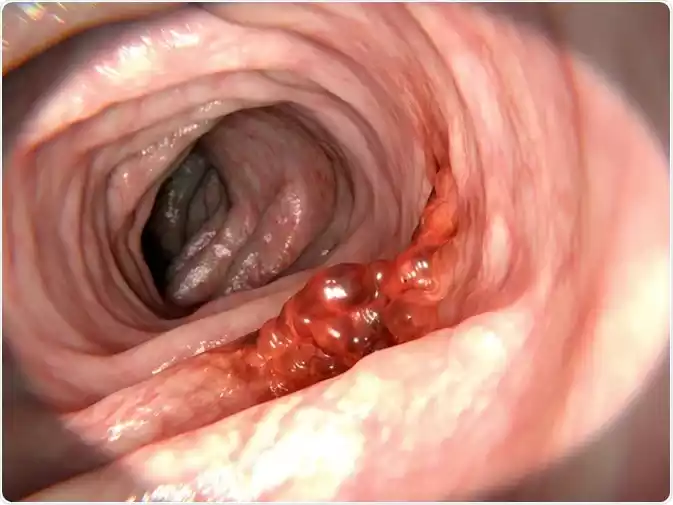
Diffuse gastric cancer is a subtype of stomach (gastric) cancer characterized by its unique pathological features and clinical behavior. In diffuse gastric cancer, cancer cells infiltrate and spread diffusely throughout the stomach wall, making it challenging to identify distinct tumor masses. One hallmark of diffuse gastric cancer is the presence of signet ring cells, which are cancer cells with a characteristic appearance under a microscope.

This subtype is often associated with a poorer prognosis compared to other gastric cancer types due to its aggressive nature and tendency to be diagnosed at more advanced stages. Understanding these characteristics is crucial for accurate diagnosis and treatment planning for individuals with diffuse gastric cancer.
Causes of Diffuse Gastric Cancer
The exact causes of diffuse gastric cancer are not fully understood, but several factors and risk factors have been associated with an increased likelihood of developing this subtype of stomach cancer. Diffuse gastric cancer is characterized by its diffuse infiltration of cancer cells throughout the stomach wall, often presenting with a signet ring cell appearance.
Some of the potential causes and risk factors for diffuse gastric cancer include:
-
- Genetic Predisposition: Hereditary Diffuse Gastric Cancer (HDGC) syndrome is a genetic condition linked to mutations in the CDH1 gene. Individuals with HDGC are at a significantly higher risk of developing diffuse gastric cancer. Family history of gastric cancer or certain other cancers may also increase the risk.
- Helicobacter pylori Infection: While H. pylori infection is more commonly associated with intestinal gastric cancer, it may also play a role in the development of diffuse gastric cancer. Chronic H. pylori infection can lead to chronic gastritis and increase the risk of stomach cancer.
- Age and Gender: Like other types of stomach cancer, diffuse gastric cancer tends to affect older individuals more frequently and is more common in men than in women.
- Dietary Factors: Diets high in salt, smoked and pickled foods, and low in fruits and vegetables have been associated with an increased risk of gastric cancer, including the diffuse subtype.
- Tobacco and Alcohol Use: Smoking and heavy alcohol consumption have been linked to an elevated risk of gastric cancer.
- Occupational Exposures: Certain occupational exposures, such as working in industries with chemical exposures or coal mining, have been associated with an increased risk of gastric cancer.
- Previous Stomach Surgery: Individuals who have had partial gastrectomy (removal of a portion of the stomach) for other reasons may have an increased risk of gastric cancer, including the diffuse subtype.
- Race and Ethnicity: Some populations, such as those in certain regions of Asia and South America, have a higher incidence of gastric cancer, including diffuse gastric cancer.
It’s essential to emphasize that while these factors may increase the risk of diffuse gastric cancer, not everyone exposed to these risk factors will develop the disease. Moreover, the exact mechanisms by which these factors contribute to the development of diffuse gastric cancer are still under investigation.
If there is a family history of gastric cancer or any concerns about the risk of diffuse gastric cancer, individuals should consider genetic counseling and screening. Additionally, early diagnosis through medical evaluation and regular check-ups is crucial for improving the outcomes of individuals with gastric cancer, including the diffuse subtype.
Symptoms of Diffuse Gastric Cancer
Diffuse gastric cancer, a subtype of stomach cancer characterized by the infiltration of cancer cells throughout the stomach wall and often a signet ring cell appearance, can manifest with various symptoms. However, it’s important to note that the symptoms of diffuse gastric cancer can be non-specific and may resemble other gastrointestinal conditions. If you experience persistent or concerning symptoms, it’s crucial to seek medical evaluation.
Common symptoms of diffuse gastric cancer may include:
-
- Abdominal Pain: Persistent or recurrent abdominal pain or discomfort, often localized in the upper abdomen.
- Early Satiety: Feeling full quickly or after consuming small amounts of food, which can contribute to unintentional weight loss.
- Nausea and Vomiting: Frequent nausea, sometimes accompanied by vomiting, especially after eating.
- Loss of Appetite: A noticeable reduction in appetite, leading to decreased food intake.
- Unexplained Weight Loss: Significant and unexplained weight loss, often associated with a decreased appetite.
- Fatigue: Ongoing fatigue or weakness, which may result from anemia due to bleeding from the stomach lining.
- Blood in Stool or Vomit: Occasional or recurrent bleeding from the stomach may lead to the presence of blood in stools (melena) or vomiting of blood (hematemesis).
- Difficulty Swallowing: Dysphagia, or difficulty swallowing, can occur when the tumor grows and obstructs the passage from the stomach to the small intestine.
- Heartburn: Persistent heartburn or gastroesophageal reflux symptoms, although less common, can be associated with diffuse gastric cancer.
- Paleness: Anemia-related symptoms, such as paleness of the skin and fatigue, can develop if the cancer causes chronic bleeding.
- Enlarged Lymph Nodes: In advanced stages, the cancer may spread to nearby lymph nodes, leading to enlarged lymph nodes in the neck, armpits, or groin.
- Ascites: In advanced cases, fluid accumulation in the abdominal cavity (ascites) may occur, leading to abdominal swelling and discomfort.
It’s important to recognize that these symptoms can vary in severity, and some individuals may experience only a subset of them. Additionally, many of these symptoms are non-specific and can be caused by various gastrointestinal conditions. Therefore, a comprehensive medical evaluation, including physical examinations, endoscopic procedures (such as gastroscopy), imaging tests, and biopsies, is necessary to diagnose diffuse gastric cancer accurately.
If you or someone you know is experiencing persistent or concerning gastrointestinal symptoms, it’s advisable to consult with a healthcare professional for a thorough evaluation and appropriate diagnostic tests. Early detection and treatment can significantly improve the prognosis for individuals with gastric cancer, including the diffuse subtype.
Comparison Table of Intestinal and Diffuse Gastric Cancer
Here’s a comparison table highlighting the key differences between Intestinal and Diffuse Gastric Cancer:
| Characteristic | Intestinal Gastric Cancer | Diffuse Gastric Cancer |
|---|---|---|
| Histological Appearance | Well-defined tumor structures | Diffuse infiltration of cells |
| Growth Pattern | Tends to form distinct masses | Infiltrates stomach wall widely |
| Pre-Malignant Changes | Often associated with intestinal metaplasia | May not be associated with specific precursors |
| Histological Features | Glandular formation in tumor tissue | Signet ring cells are common |
| Clinical Presentation | May cause indigestion, weight loss, pain | Often presents with vague symptoms, such as abdominal discomfort and bloating |
| Diagnosis | Endoscopy and biopsy are used to identify the characteristic appearance | May require multiple biopsies due to diffuse nature |
| Treatment Approaches | Surgery, chemotherapy, and radiation therapy are common treatments | Surgery may be challenging due to diffuse infiltration; chemotherapy often used |
| Prognosis | Generally associated with a better prognosis compared to diffuse type | Often diagnosed at advanced stages, leading to poorer prognosis |
| Molecular Features | May have specific genetic alterations, such as microsatellite instability | May have unique molecular markers, like CDH1 gene mutations in some cases |
| Incidence | Less common subtype of gastric cancer | Less common compared to intestinal type |
| Survival Rates | Tends to have better survival rates compared to diffuse type | Tends to have lower survival rates due to late-stage diagnosis |
Individual cases of gastric cancer can vary, and this table provides a general overview of the differences between these two subtypes. Diagnosis and treatment decisions should always be made in consultation with healthcare professionals based on the specific characteristics of each patient’s case.
How to diagnosis of Intestinal and Diffuse Gastric Cancer
The diagnosis of both intestinal and diffuse gastric cancer involves a combination of clinical assessments, imaging studies, endoscopic procedures, and histopathological examination. Here’s an overview of the diagnostic process for these gastric cancer subtypes:
Diagnosis of Intestinal Gastric Cancer:
- Clinical Evaluation:
- The diagnostic process often begins with a thorough medical history and physical examination to assess symptoms and risk factors.
- Family history of gastric cancer or other related conditions may be assessed.
- Endoscopy (Gastroscopy):
- Upper endoscopy is a crucial step in diagnosing gastric cancer. A thin, flexible tube with a camera on the end (endoscope) is inserted through the mouth and into the stomach.
- The endoscope allows direct visualization of the stomach lining, enabling the detection of suspicious lesions or tumors.
- Biopsy:
- During endoscopy, tissue samples (biopsies) are obtained from any suspicious areas. Biopsies are essential for confirming the presence of cancer and determining its type and stage.
- Histopathological examination of the biopsy samples helps identify the characteristic features of intestinal gastric cancer.
- Imaging Studies:
- Complementary imaging tests such as computed tomography (CT) scans and positron emission tomography (PET) scans may be performed to evaluate the extent of tumor spread and assess lymph node involvement.
- Staging:
- After confirmation of gastric cancer, staging is conducted to determine the extent of the disease and its spread. Staging helps guide treatment decisions.
Diagnosis of Diffuse Gastric Cancer:
- Clinical Evaluation:
- Similar to intestinal gastric cancer, the diagnostic process begins with a comprehensive medical history, physical examination, and an assessment of symptoms and risk factors.
- Endoscopy (Gastroscopy):
- Upper endoscopy is performed to visualize the stomach lining and identify any suspicious areas.
- However, diffuse gastric cancer often presents as thickening of the stomach wall with no distinct masses, making it challenging to detect through endoscopy.
- Biopsy:
- Biopsies are crucial for diagnosing diffuse gastric cancer. Multiple biopsies from various areas of the stomach may be required due to the diffuse and infiltrative nature of the cancer.
- Histopathological examination of the biopsies reveals the presence of signet ring cells or other characteristic features.
- Imaging Studies:
- CT scans, PET scans, and other imaging studies help determine the extent of tumor infiltration and identify any metastases or lymph node involvement.
- Staging:
- Staging is essential to determine the stage of diffuse gastric cancer and guide treatment decisions.
Once the diagnosis and staging are complete, a multidisciplinary team of healthcare professionals, including oncologists and surgeons, will discuss treatment options, which may include surgery, chemotherapy, radiation therapy, targeted therapies, and immunotherapy. Early diagnosis and accurate staging are crucial for tailoring treatment plans to each patient’s specific needs and improving outcomes.
Treatment for Intestinal and Diffuse Gastric Cancer
The treatment for both intestinal and diffuse gastric cancer typically involves a multidisciplinary approach, tailored to the individual patient’s stage of cancer, overall health, and specific circumstances. Treatment options may include surgery, chemotherapy, radiation therapy, targeted therapies, and immunotherapy. The choice of treatment depends on factors such as the cancer’s stage, location, and molecular characteristics.
Here is an overview of treatment options for both types of gastric cancer:
Treatment for Intestinal Gastric Cancer:
- Surgery: Surgery is often the primary treatment for localized intestinal gastric cancer. The extent of surgery depends on the cancer’s stage and location and may involve one of the following procedures:
- Subtotal Gastrectomy: Removal of the part of the stomach containing the tumor.
- Total Gastrectomy: Removal of the entire stomach if the cancer is more extensive.
- Lymph Node Dissection: Removal of nearby lymph nodes to assess cancer spread.
- Chemotherapy: Chemotherapy may be recommended before surgery (neoadjuvant chemotherapy) to shrink the tumor or after surgery (adjuvant chemotherapy) to eliminate any remaining cancer cells.
- Radiation Therapy: Radiation therapy may be used in combination with chemotherapy (chemoradiation) to enhance the effectiveness of treatment, particularly in locally advanced cases.
- Targeted Therapies: Some cases of gastric cancer may involve specific molecular alterations. Targeted therapies are drugs that target these specific genetic changes to inhibit cancer growth.
- Immunotherapy: Immunotherapy drugs like checkpoint inhibitors may be used to stimulate the immune system’s response against cancer cells.
Treatment for Diffuse Gastric Cancer:
Treatment for diffuse gastric cancer is similar to that for intestinal gastric cancer, but it can be more challenging due to its diffuse infiltrative nature. Here are the treatment options:
- Surgery: Surgical resection may still be attempted in cases where the tumor is localized and resectable. However, due to the diffuse infiltration, complete removal can be challenging.
- Chemotherapy: Chemotherapy is often the primary treatment for diffuse gastric cancer, either before or after surgery, depending on the stage and extent of the disease.
- Radiation Therapy: Radiation therapy may be used in combination with chemotherapy for localized tumors or to alleviate symptoms in advanced cases.
- Targeted Therapies: Targeted therapies may be considered if specific molecular alterations are identified in the tumor.
- Immunotherapy: Immunotherapy drugs are being explored in clinical trials for diffuse gastric cancer, although their effectiveness in this subtype is an active area of research.
- Palliative Care: In advanced or metastatic cases where curative treatment is not possible, palliative care focuses on managing symptoms, improving quality of life, and providing supportive care.
It’s crucial for individuals with gastric cancer, whether intestinal or diffuse, to consult with a multidisciplinary team of healthcare professionals, including oncologists, surgeons, and gastroenterologists, to determine the most appropriate treatment plan based on their specific diagnosis and circumstances. Treatment decisions should be personalized, taking into account the cancer’s stage, the patient’s overall health, and their preferences. Clinical trials may also offer promising new treatment options for gastric cancer, and patients are encouraged to discuss participation in these trials with their healthcare team.
Conclusion
Intestinal and Diffuse Gastric Cancer are distinct subtypes of stomach cancer, each presenting unique challenges in diagnosis and treatment. Intestinal gastric cancer is characterized by well-defined tumor structures and is often associated with pre-malignant changes, while diffuse gastric cancer displays diffuse infiltration of cancer cells and signet ring cell appearance.
Early diagnosis and tailored treatment plans, including surgery, chemotherapy, targeted therapies, and immunotherapy, are essential for improving outcomes. However, both subtypes can be aggressive, underscoring the importance of timely medical evaluation and a multidisciplinary approach to care. Advances in research and personalized treatment strategies offer hope for better outcomes for individuals affected by these challenging malignancies.