Glaucoma and Trachoma are both eye conditions but differ significantly in their causes, symptoms, and treatment. Glaucoma is primarily a degenerative condition often linked to elevated intraocular pressure that damages the optic nerve, leading to vision loss. It is generally more prevalent in older adults and those with a family history of the disease. Trachoma, on the other hand, is an infectious disease caused by the bacterium Chlamydia trachomatis.
Common in developing countries, it spreads through direct and indirect contact and can result in blindness if not treated. While glaucoma management focuses on lowering eye pressure through medication, laser therapy, or surgery, trachoma is usually treated with antibiotics and public health interventions like improved sanitation.
What is Glaucoma?
Glaucoma is a medical condition characterized by damage to the optic nerve, often resulting from elevated intraocular pressure (IOP) within the eye. This damage can lead to progressive, irreversible vision loss, starting with the loss of peripheral vision and potentially progressing to blindness if left untreated. Glaucoma is one of the leading causes of blindness worldwide, and its onset is often asymptomatic, making early detection through regular eye examinations crucial for effective management.
Types of Glaucoma
Glaucoma is a complex group of eye disorders that share a common feature: damage to the optic nerve, often accompanied by elevated intraocular pressure (IOP). Here are some common types of glaucoma:
Open-Angle Glaucoma
- Description: This is the most common form of glaucoma, accounting for about 90% of cases.
- Symptoms: Usually asymptomatic in the early stages, with gradual peripheral vision loss.
- Causes: Blocked or poorly draining trabecular meshwork, leading to increased IOP.
- Treatment: Eye drops to reduce IOP, laser trabeculoplasty, or surgical procedures like trabeculectomy.
Angle-Closure Glaucoma
- Description: Less common but more urgent, this type occurs when the angle between the cornea and iris closes abruptly.
- Symptoms: Sudden eye pain, nausea, halos around lights, and vision loss.
- Causes: Rapid rise in IOP due to blocked drainage canals.
- Treatment: Emergency medical intervention, including medications and laser peripheral iridotomy to relieve IOP.
Normal-Tension Glaucoma
- Description: Optic nerve damage occurs even though the IOP is within the “normal” range.
- Symptoms: Similar to open-angle glaucoma but can progress more unpredictably.
- Causes: Unknown; possibly related to poor blood flow to the optic nerve.
- Treatment: Similar to treatments for open-angle glaucoma, focusing on lowering IOP even further.
Congenital Glaucoma
- Description: Present at birth or developing in the first few years of life.
- Symptoms: Excessive tearing, sensitivity to light, and cloudy or enlarged eyes.
- Causes: Developmental issues with the eye’s drainage system.
- Treatment: Surgical intervention is often necessary, and medications may be used.
Secondary Glaucoma
- Description: Caused by another eye or systemic condition.
- Symptoms: Depends on the underlying condition.
- Causes: Conditions like uveitis, diabetes, or trauma can lead to elevated IOP.
- Treatment: Treat the underlying condition and manage IOP similarly to primary glaucoma.
Each type of glaucoma requires specialized diagnosis and treatment strategies, often involving a combination of medication, laser treatment, and surgical procedures. Regular eye examinations are crucial for early detection and effective management.
Causes of Glaucoma
The causes of glaucoma are not fully understood, but there are several risk factors and underlying mechanisms that are commonly associated with the condition. Elevated intraocular pressure (IOP) is often a significant factor, although not everyone with elevated IOP will develop glaucoma.
Here are some common causes and risk factors:
Causes and Mechanisms
- Increased Intraocular Pressure (IOP): The most commonly cited factor, increased pressure inside the eye can result from poor drainage of aqueous humor, the eye’s internal fluid.
- Blocked or Poorly Functioning Drainage Channels: The eye has a drainage system (trabecular meshwork) that allows the aqueous humor to flow out. Blockage or dysfunction can result in elevated IOP.
- Reduced Blood Flow to Optic Nerve: In cases of normal-tension glaucoma, reduced blood flow to the optic nerve may play a role, even when IOP is not elevated.
- Ocular or Systemic Conditions: Conditions like uveitis, diabetes, or hypertension may contribute to the onset of secondary glaucoma.
- Ocular Trauma: Physical injury to the eye can lead to traumatic glaucoma, either immediately after the injury or years later.
- Drug-Induced: Certain medications like corticosteroids can elevate IOP and thus increase the risk of developing glaucoma.
Risk Factors
- Age: Glaucoma risk increases with age, particularly for individuals over 60.
- Family History: A family history of glaucoma increases one’s risk.
- Ethnicity: Certain ethnic groups, such as people of African or Hispanic descent, are at higher risk.
- Other Medical Conditions: Diabetes, high blood pressure, and heart disease are sometimes considered risk factors for glaucoma.
- High Myopia: Extremely nearsighted individuals have a higher risk of developing glaucoma.
- Eye Anatomy: Features like a thin cornea can be risk factors for developing the disease.
- Previous Eye Surgery or Injury: A history of eye surgeries or injuries can be a risk factor for secondary glaucoma.
One or more risk factors does not mean you will definitely develop glaucoma, but it does increase your risk. Regular eye examinations are crucial for early detection and management, particularly if you have multiple risk factors.
Symptoms of Glaucoma
The symptoms of glaucoma can vary depending on the type and stage of the condition. Below are the symptoms commonly associated with different types of glaucoma:
Open-Angle Glaucoma
- Early Stages: Often asymptomatic; no noticeable change in vision.
- Later Stages: Gradual loss of peripheral vision, usually in both eyes, which can progress to tunnel vision.
Angle-Closure Glaucoma
- Acute Episodes: Sudden and severe eye pain, redness of the eye, blurred vision, halos around lights, nausea, and vomiting.
- Chronic Form: More gradual onset; symptoms may be milder but similar to those of acute angle-closure glaucoma.
Normal-Tension Glaucoma
- Early Stages: Generally asymptomatic or very subtle symptoms.
- Later Stages: Loss of peripheral vision and possibly other vision problems, although the pattern might be different from open-angle glaucoma.
Congenital Glaucoma
- Infancy: Excessive tearing, light sensitivity, cloudy eyes, and enlarged eyes.
Secondary Glaucoma
- Symptoms vary depending on the underlying condition that is causing the glaucoma but may include any of the symptoms associated with primary forms of glaucoma.
Because early-stage glaucoma is often asymptomatic, regular eye examinations are crucial for early detection and management of the disease. Detecting glaucoma in its early stages allows for more effective treatment options that can slow or halt the progression of the disease. If you experience any symptoms of glaucoma, particularly sudden changes in vision or eye pain, seek medical attention immediately.
What is Trachoma?
Trachoma is an infectious eye disease caused by the bacterium Chlamydia trachomatis. It is a leading cause of preventable blindness worldwide and is particularly prevalent in developing countries with poor sanitation and limited access to clean water. The condition is characterized by inflammation of the conjunctiva, leading to symptoms such as itchy, irritated eyes, and discharge. If left untreated, trachoma can lead to scarring of the cornea and eventually cause irreversible blindness.

The disease is transmitted through direct or indirect contact with infected eye, nose, or throat secretions, as well as via contaminated objects and flies. Treatment often involves antibiotics and sometimes surgery for more advanced cases. Public health measures, such as improved sanitation and hygiene practices, are crucial for prevention.
Types of Trachoma
Trachoma is a bacterial infection of the eye caused by Chlamydia trachomatis. It is often categorized based on the clinical presentation and stage of the disease. The World Health Organization (WHO) has simplified this into a grading system known as the “FPC grading system,” which consists of the following categories:
Follicular Trachoma (TF)
- Description: The presence of five or more follicles (small bumps) on the upper tarsal conjunctiva.
- Symptoms: Irritation, itchiness, and tearing.
- Treatment: Antibiotics, usually azithromycin or tetracycline.
Inflammatory Trachoma (TI)
- Description: Severe inflammation covering more than half of the deep tarsal vessels.
- Symptoms: Red, swollen, painful eyes, and discharge.
- Treatment: Antibiotics and sometimes topical steroid to control inflammation.
Cicatricial Trachoma (TS)
- Description: Scarring on the tarsal conjunctiva.
- Symptoms: Scarring can lead to deformities like entropion (inward turning of eyelids).
- Treatment: Surgical intervention may be necessary to prevent further complications.
Trichiasis (TT)
- Description: In-turning of the eyelashes due to scarring, which causes them to rub against the cornea.
- Symptoms: Pain, tearing, and eventual corneal damage.
- Treatment: Surgery to correct eyelash position.
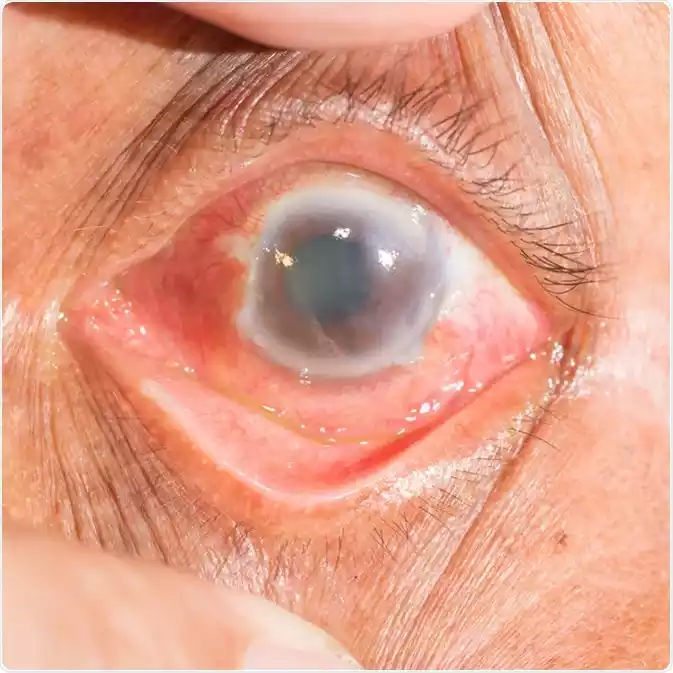
Corneal Opacity (CO)
- Description: Advanced stage where corneal scarring and opacity occur.
- Symptoms: Reduced vision or blindness.
- Treatment: Corneal transplant in extreme cases, although this is often not feasible in areas where trachoma is endemic.
Treatment strategies for trachoma are often summarized as the SAFE strategy: Surgery (for trichiasis), Antibiotics (to treat active infection), Facial cleanliness (to reduce transmission), and Environmental improvements (to reduce the breeding sites for flies that transmit the bacteria).
Differentiating between these types and stages is critical for effective treatment and prevention of complications. Public health measures play a significant role in controlling the spread of the disease, particularly in endemic areas.
Causes of Trachoma
Trachoma is caused by infection with the bacterium Chlamydia trachomatis. This bacterium infects the conjunctiva, which is the mucous membrane that covers the front of the eye and lines the inside of the eyelids. The infection can spread through various means, and certain environmental and social factors can facilitate its transmission. Here are some key causes and contributing factors:
Direct and Indirect Transmission
- Direct Contact: Person-to-person transmission through eye, nose, or throat secretions.
- Fomites: Indirect contact with infected objects like towels, clothing, or bedding can also spread the infection.
- Flies: The bacterium can also be spread by flies that have been in contact with eye or nose secretions from an infected person.
Environmental Factors
- Poor Sanitation: Lack of access to clean water and sanitation facilities can facilitate the spread of the bacterium.
- Crowding: Overcrowded living conditions make it easier for the disease to spread.
- Limited Access to Healthcare: Limited availability of medical services can contribute to the spread of trachoma, as treatment is less likely to be administered early.
Social and Economic Factors
- Poverty: Poor communities are at higher risk, as they may lack the resources to maintain proper hygiene or access healthcare.
- Gender: Women and children are more often affected, possibly due to their role in childcare and closer contact with infected individuals.
- Local Customs and Practices: Certain social practices, such as communal use of washcloths, may also contribute to transmission.
Geographic Factors
- Climate: Trachoma is more prevalent in hot, dry climates where flies that spread the disease are more abundant.
- Endemic Areas: People living in areas where trachoma is endemic are at higher risk of getting infected.
Understanding these causes and contributing factors is essential for effective public health interventions to control and eventually eliminate trachoma. The World Health Organization recommends a multi-faceted approach called the SAFE strategy (Surgery, Antibiotics, Facial cleanliness, and Environmental improvements) to control the spread of this disease.
Symptoms of Trachoma
Trachoma, caused by the bacterium Chlamydia trachomatis, affects the conjunctiva of the eyes. The symptoms evolve as the disease progresses through its stages. Here are the common symptoms associated with different stages of trachoma:
Early Stages:
- Follicular Trachoma (TF):
- Presence of small, white follicles (bumps) on the inner surface of the upper eyelid.
- Redness and irritation in the eyes.
- Itchiness and mild pain.
- Discharge from the eyes.
- Intense Inflammatory Trachoma (TI):
- Severe inflammation of the upper eyelid.
- Swollen eyelids.
- Pain, especially when exposed to bright light.
- Increased tearing.
Advanced Stages:
- Scarring (TS):
- Scars on the inner surface of the upper eyelid. They may appear as white lines or bands.
- The eyelid may become distorted due to scarring, which can lead to further complications.
- Trichiasis (TT):
- Eyelashes turn inwards because of scarring and lid deformities.
- In-turned eyelashes rub against the eyeball, causing pain and discomfort.
- Continuous abrasion can lead to corneal damage.
- Corneal Opacity (CO):
- The cornea becomes cloudy and opaque due to repeated infections and continuous abrasion from in-turned eyelashes.
- Reduced vision or complete blindness.
Early detection and treatment of trachoma can prevent progression to the more severe stages. It’s important to trachoma is highly contagious, especially in its early stages. Proper hygiene practices, prompt treatment, and health education can help control its spread, particularly in endemic areas. If someone suspects they have trachoma or exhibits any of the mentioned symptoms, they should seek medical attention promptly.
Comparison Table of Glaucoma and Trachoma
Certainly, here’s a comparison table that highlights key differences between Glaucoma and Trachoma:
| Criteria | Glaucoma | Trachoma |
|---|---|---|
| Cause | Elevated intraocular pressure, unclear etiology | Infection by Chlamydia trachomatis |
| Transmission | Non-communicable | Communicable through direct and indirect contact, flies |
| Common Types | Open-Angle, Angle-Closure, Normal-Tension, Secondary | Follicular, Inflammatory, Scarring, Trichiasis, Corneal Opacity |
| Early Symptoms | Often asymptomatic in open-angle; sudden pain in angle-closure | Eye irritation, redness, follicles, discharge |
| Late Symptoms | Peripheral vision loss, tunnel vision | Scarring, eyelid deformation, vision loss or blindness |
| Diagnostic Tests | Tonometry, Visual field testing, OCT scan | Clinical examination, sometimes laboratory tests |
| Treatment | Eye drops, laser surgery, traditional surgery | Antibiotics, sometimes surgery for late-stage complications |
| Prevalence | More common in developed countries, older adults | More common in developing countries, affects all age groups |
| Risk Factors | Age, family history, ethnicity, high IOP | Poor sanitation, crowded living conditions, flies |
| Prevention | Regular eye screenings | Improved hygiene, sanitation, health education |
| Potential Complications | Blindness, optic nerve damage | Scarring, corneal damage, blindness |
This table summarizes some of the key features and differences between glaucoma and trachoma but is not exhaustive. Each condition has its own complexities and may require specialized diagnosis and treatment.
Diagnosis of Glaucoma and Trachoma
Diagnosis of Glaucoma and Trachoma involves different approaches, given that they are distinct conditions with varying symptoms, causes, and risk factors.

Below is an overview of how each is typically diagnosed.
Diagnosis of Glaucoma
- Comprehensive Eye Exam: Often includes measuring intraocular pressure (IOP) using tonometry, examining the optic nerve head, and assessing visual fields.
- Visual Field Test: A perimetry test may be performed to check for areas of vision loss. This is especially important for diagnosing open-angle glaucoma.
- Optical Coherence Tomography (OCT): This is a non-invasive imaging test that can provide detailed images of the optic nerve and measure its thickness.
- Gonioscopy: This involves examining the drainage angle of the eye to determine if it’s open or closed, helping to distinguish between open-angle and angle-closure glaucoma.
- Pachymetry: Measures the thickness of the cornea, which can influence IOP readings and provide additional information about glaucoma risk.
- Medical History and Risk Assessment: Family history of glaucoma, previous eye injuries, and other risk factors are also considered.
Diagnosis of Trachoma
- Clinical Examination: Often the first step in diagnosis, looking for signs like eye discharge, inflammation, and the presence of follicles or scarring on the inside of the upper eyelid.
- Microscopic Examination: In some cases, swabs from the conjunctiva may be examined under a microscope or sent for laboratory testing to confirm the presence of Chlamydia trachomatis.
- Nucleic Acid Amplification Tests (NAATs): These are highly sensitive and specific tests that can identify bacterial DNA or RNA. However, they are rarely used in field settings due to cost and equipment constraints.
- Serological Tests: These blood tests can detect antibodies to Chlamydia trachomatis, but they are generally not used for diagnosis since they can’t distinguish between current and past infections.
- Community Surveys: In endemic areas, community-level surveys may be conducted to assess the prevalence of trachoma and guide mass treatment strategies.
- Assessment of Environmental Risk Factors: In endemic areas, factors like water supply, sanitation, and fly density may be assessed.
Early diagnosis and treatment are crucial for both conditions to prevent irreversible damage and complications. Therefore, regular eye check-ups are advised, especially for those who are at higher risk.
Treatment Options for Glaucoma and Trachoma
Treatment options for Glaucoma and Trachoma are distinct, owing to the differences in their underlying causes, stages, and symptoms. Below are some of the common treatment modalities for each condition.
Treatment Options for Glaucoma:
- Eye Drops: The first line of treatment often involves medicated eye drops that either decrease the production of aqueous humor or increase its drainage, thereby lowering intraocular pressure (IOP).
- Prostaglandin analogs: Increase drainage
- Beta-blockers: Reduce aqueous humor production
- Carbonic anhydrase inhibitors: Reduce aqueous humor production
- Rho kinase inhibitors: Increase drainage
- Alpha agonists: Reduce aqueous humor production and increase drainage
- Laser Therapy: Used in various forms, such as:
- Selective Laser Trabeculoplasty (SLT): For open-angle glaucoma
- Laser Peripheral Iridotomy (LPI): For angle-closure glaucoma
- Cyclophotocoagulation: Targets the ciliary body to reduce aqueous humor production
- Surgical Procedures: When medication and laser treatments are not effective or suitable.
- Trabeculectomy: Creating a new drainage pathway
- Glaucoma Drainage Devices: Implanting a tiny tube to drain fluid
- Minimally Invasive Glaucoma Surgery (MIGS): Newer techniques that are less invasive
- Oral Medications: Carbonic anhydrase inhibitors may be prescribed in pill form but are generally reserved for severe or acute cases due to side effects.
Treatment Options for Trachoma:
- Antibiotics: The cornerstone of trachoma treatment.
- Azithromycin: Single oral dose
- Tetracycline Eye Ointment: Applied to the eyes for several weeks
- Surgery: For advanced stages like trichiasis or eyelid deformities.
- Eyelid Rotation Surgery: To correct the position of in-turned eyelashes
- Facial Cleanliness: Encouraged to reduce transmission, particularly among children.
- Environmental Sanitation: Improved access to clean water and sanitation facilities to reduce transmission.
- Community-Based Treatment: In endemic areas, mass drug administration (MDA) of antibiotics may be undertaken to reduce community-wide prevalence.
- Public Health Education: Teaching proper hygiene and sanitation practices to affected communities.
For both conditions, early detection and timely intervention are key to preventing irreversible damage. Glaucoma treatment is generally lifelong and aimed at lowering IOP to prevent further optic nerve damage. Trachoma treatment aims to cure the infection and prevent complications. Always consult healthcare professionals for accurate diagnosis and appropriate treatment.
Prevention for Glaucoma and Trachoma
Prevention strategies for Glaucoma and Trachoma vary due to the distinct nature of each disease—glaucoma being largely non-communicable and related to factors like age and genetics, while trachoma is an infectious disease often tied to poor sanitation and hygiene.
Prevention for Glaucoma:
- Regular Eye Exams: The most effective way to prevent glaucoma or mitigate its effects is through early detection, made possible by regular, comprehensive eye exams, especially for those at higher risk.
- Manage Risk Factors: Keeping conditions like diabetes and high blood pressure under control can help in reducing the risk.
- Lifestyle Changes: Some studies suggest that regular exercise can help lower eye pressure. However, consult with an eye care specialist for exercise guidelines.
- Avoid Excessive Fluid Intake in Short Periods: Large fluid intakes in a short time can temporarily increase eye pressure.
- Educate and Create Awareness: Knowledge of family history and the risks associated with glaucoma can lead to earlier screenings and preventive care.
- Eye Protection: Use protective eyewear to prevent eye injuries that could lead to secondary glaucoma.
- Medication Compliance: If you’re already diagnosed with elevated eye pressure or glaucoma, following the medication regimen strictly can prevent progression.
Prevention for Trachoma:
- Improving Sanitation: Access to clean water and improved sanitation can significantly reduce the transmission of the bacteria causing trachoma.
- Face Washing: Regular face washing, especially among children, removes eye discharges that can contain bacteria.
- Use of Latrines: Encouraging the use of latrines reduces breeding grounds for flies that can transmit the disease.
- Fly Control: Reducing fly populations through environmental changes and insecticides can cut down on transmission.
- Community Education: Educating communities about the importance of hygiene and sanitation can reduce the incidence of trachoma.
- Mass Drug Administration (MDA): In endemic areas, mass distribution of antibiotics like azithromycin can help prevent the spread of infection.
- Isolation of Infected Individuals: Limiting close contact, sharing of personal items, and improved hand hygiene can reduce the spread of active infection.
- Regular Eye Examinations: In endemic areas, frequent eye examinations can help in early diagnosis and treatment, reducing complications.
Both glaucoma and trachoma require distinct preventive approaches but share the common factor of benefitting significantly from early detection and treatment. Preventive measures for glaucoma are often more focused on individual health, while those for trachoma are often community-based, given its infectious nature. Always consult healthcare professionals for an accurate diagnosis and appropriate preventive measures.
Current Research and Future Outlook
As of my last update in January 2022, considerable efforts are being made in both glaucoma and trachoma research to better understand these diseases, improve diagnostic methods, and develop more effective treatments. Below are some key areas of research and what the future might hold for each:
Glaucoma
- Biomarkers: Research is ongoing to identify specific biomarkers that can provide early indications of glaucoma, potentially allowing for more timely intervention.
- Gene Therapy: Efforts are underway to understand the genetic factors associated with glaucoma and how gene therapy might be used for treatment.
- Advanced Imaging Techniques: New imaging methods may offer a more detailed view of the optic nerve and retina, aiding in early detection and monitoring.
- New Drug Formulations: There is active research into new medications, including sustained-release formulations that could reduce the frequency of eye drops.
- Neuroprotection: Studies are examining if various compounds can protect the optic nerve from damage, which is a central feature of glaucoma.
- Telemedicine: In light of the COVID-19 pandemic, there’s an increasing focus on remote monitoring technologies for glaucoma patients.
Trachoma
- Vaccine Development: There is ongoing research into developing a vaccine for trachoma, which could be a game-changer for disease eradication.
- Alternative Antibiotics: With antibiotic resistance a growing concern, research is exploring alternative antibiotic regimens.
- Improved Diagnostic Tests: Efforts are being made to develop quick and cost-effective diagnostic tests, which would be especially useful in low-resource settings.
- Surgical Techniques: Research continues on improving surgical interventions for the later stages of trachoma to optimize outcomes and reduce recurrence.
- Health Economics Studies: Research is exploring the cost-effectiveness of mass drug administration vs. targeted treatments, which could influence future public health strategies.
- Environmental Interventions: Studies are looking at the impact of water, sanitation, and hygiene (WASH) interventions on trachoma transmission.
Future Outlook
For Glaucoma, the aim is to move toward early diagnosis and intervention, possibly even preemptive treatment for those at high risk. More convenient and less invasive treatment options are also on the horizon.
For Trachoma, the World Health Organization has targeted the disease for elimination as a public health problem by 2030. Success will likely depend on a combination of medical treatment, surgical intervention, and sustained improvements in public health infrastructure.
Given the rapid pace of medical research, it is hoped that new breakthroughs will significantly improve the prevention, diagnosis, and treatment of both conditions in the coming years.
Final Thoughts
Glaucoma and Trachoma are both eye diseases that can lead to irreversible vision loss if not properly managed. While glaucoma is primarily associated with elevated intraocular pressure and often targets older populations, trachoma is an infectious disease caused by Chlamydia trachomatis and is prevalent in areas with poor sanitation and hygiene. Glaucoma management focuses on lowering eye pressure through medications, laser treatments, or surgery, while trachoma treatment involves antibiotics and may require surgical intervention in advanced cases.
Both conditions underscore the importance of early detection and intervention, with prevention strategies varying significantly due to their different etiologies. Advances in medical research continue to refine our understanding and treatment of these conditions, offering hope for more effective interventions in the future.