Omphalocele and Gastroschisis are both congenital abdominal wall defects observed in newborns, but they present distinct differences in terms of location, appearance, and associated risks. Omphalocele is characterized by the protrusion of abdominal organs into an external sac at the base of the umbilical cord. This sac is typically covered by a thin, translucent membrane.
On the other hand, Gastroschisis manifests as an abdominal wall defect usually to the right of the umbilical cord, with intestines herniating outside without any protective sac. Early detection and understanding of these conditions are crucial for effective prenatal care and postnatal management.
Definition of Omphalocele
Omphalocele is a congenital defect in which some of the abdominal organs (such as the intestines, liver, and occasionally other organs) protrude from the abdominal cavity and lie outside the body in a thin, sac-like structure. This defect is located at the base of the umbilical cord, and the protruding organs are covered by a translucent membrane made up of peritoneum (the lining of the abdominal cavity) and amnion (the innermost layer of the placenta).

The size of an omphalocele can vary, with some being small and containing only a portion of the intestines, while others are larger and include multiple organs. It’s essential to differentiate omphalocele from other abdominal wall defects, as its management and associated anomalies can differ.
Definition of Gastroschisis
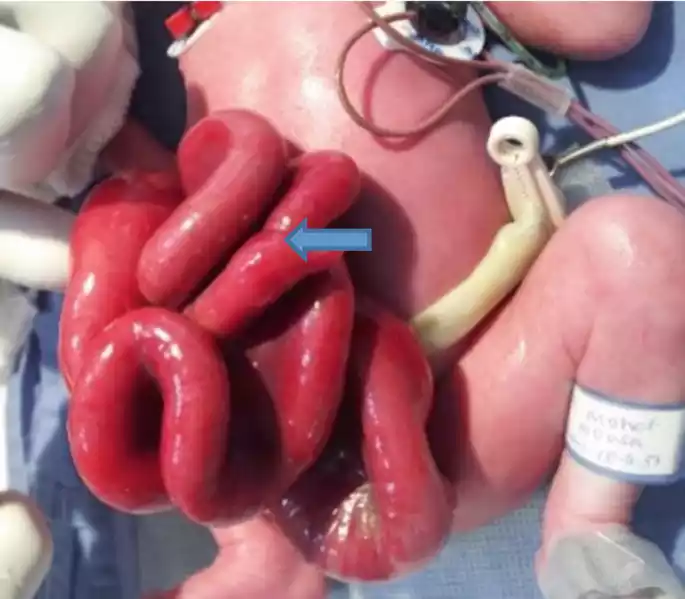
Gastroschisis is a congenital abdominal wall defect characterized by the protrusion of intestines, and occasionally other abdominal organs, directly into the amniotic fluid without the protection of a sac. This defect is typically located to the right of the umbilical cord. Unlike omphalocele, the exposed organs in gastroschisis are not covered by a membrane.
The exact cause of gastroschisis is unknown, but it tends to occur more frequently in younger mothers. Quick surgical intervention after birth is typically required to protect the exposed intestines from further damage and to place them back inside the abdominal cavity.
Comparison Table of Omphalocele and Gastroschisis
Here’s a comparison table for Omphalocele and Gastroschisis:
| Feature | Omphalocele | Gastroschisis |
|---|---|---|
| Location of Defect | Base of the umbilical cord | Typically to the right of the umbilical cord |
| Appearance | Protruding organs are in a sac | Exposed organs without a sac |
| Covering Membrane | Yes (peritoneum and amnion) | No |
| Commonly Affected Organs | Intestines, liver, and sometimes other organs | Mostly intestines, occasionally other organs |
| Associated Anomalies | Often (e.g., cardiac defects, chromosomal anomalies) | Rarely associated with other anomalies |
| Etiological Factors | Sometimes linked to genetic syndromes | Often seen in pregnancies with younger mothers, exact cause unknown |
| Incidence | Less common than gastroschisis | More common than omphalocele |
| Treatment | Varies based on size; can range from observation to surgical intervention | Almost always requires surgical intervention post-birth |
This table provides a clear comparison between Omphalocele and Gastroschisis. The differences highlighted can guide healthcare professionals in diagnosis, management, and patient counseling.
Etiology and Risk Factors
Etiology and risk factors for both Omphalocele and Gastroschisis:
1. Omphalocele:
Etiology:
- The exact cause is not always known, but omphalocele may be associated with chromosomal abnormalities and genetic syndromes.
Risk Factors:
- Advanced Maternal Age: Older mothers might have a slightly increased risk.
- Use of certain medications or drugs during early pregnancy.
- Chromosomal Anomalies: Such as Trisomy 18 (Edward’s syndrome) or Trisomy 13 (Patau syndrome).
- Multiple pregnancies: Twins, triplets, etc.
- History of Omphalocele: If parents had the condition or had another child with it.
- Certain maternal conditions: Like diabetes, obesity, and some infections during pregnancy.
2. Gastroschisis:
Etiology:
- The exact cause is largely unknown.
- Some researchers believe it might be due to a vascular accident (a problem with blood flow) during embryonic development.
Risk Factors:
- Young Maternal Age: Mothers under the age of 20 are considered to have a higher risk.
- Tobacco use: Mothers who smoke or use tobacco products during pregnancy.
- Recreational drug use: Especially early in pregnancy.
- Alcohol consumption: During early pregnancy.
- Certain medications: Some studies suggest an association with medications taken early in pregnancy, such as pain relievers, but the evidence is not strong.
- Environmental factors: Exposure to certain chemicals or infections during early pregnancy.
While both conditions have certain risk factors associated with them, it’s essential to remember that many babies born with Omphalocele or Gastroschisis don’t have any known risk factors. Regular prenatal care and screening can help detect these conditions early on, allowing for better management and outcomes for both mother and baby.
Clinical Presentation of Omphalocele and Gastroschisis
The clinical presentation of Omphalocele and Gastroschisis is distinct, making them relatively straightforward to differentiate upon visual examination:
1. Omphalocele:
- Visible Defect at Birth: Omphalocele is easily recognizable as a defect at the base of the umbilical cord.
- Size Variation: The defect can vary in size. Smaller omphaloceles may contain only a part of the intestines, while larger ones may also include the liver, stomach, and other organs.
- Protective Sac: The protruding organs are covered by a translucent sac made up of peritoneum (lining of the abdominal cavity) and amnion (innermost layer of the placenta).
- Associated Anomalies: Often, there might be other anomalies present. Babies with omphalocele may have cardiac defects, chromosomal abnormalities, or skeletal malformations.
2. Gastroschisis:
- Visible Defect at Birth: Gastroschisis is characterized by a defect in the abdominal wall, usually to the right of the umbilical cord.
- Exposed Intestines: The intestines are typically herniated outside the abdominal cavity. They appear exposed without any protective covering sac.
- Swollen and Matted Appearance: Due to direct contact with amniotic fluid, the intestines often appear irritated, swollen, and might be matted together.
- Isolated Defect: Unlike omphalocele, gastroschisis is usually an isolated defect, meaning it typically isn’t associated with other syndromes or chromosomal abnormalities.
The early identification of the defect, either through prenatal ultrasound or immediately after birth, allows healthcare providers to plan necessary interventions and care. This can significantly improve the outcomes for the newborns.
Complications of Omphalocele and Gastroschisis
Both Omphalocele and Gastroschisis can lead to various complications if not managed promptly and effectively. Let’s delve into the potential complications associated with each condition:
1. Omphalocele:
- Respiratory Distress: Due to the abdominal organs occupying space in the chest, lung development might be compromised, leading to respiratory issues in the newborn.
- Infection: The thin sac covering the organs is susceptible to rupture or tears, leading to a risk of infections.
- Associated Anomalies: Many babies with omphalocele have associated congenital anomalies, especially of the heart.
- Growth and Nutritional Issues: Depending on the severity, there might be challenges related to feeding and nutrition.
- Bowel Obstruction: Herniated bowel loops may become twisted or compressed.
- Liver Complications: If the liver is involved in the herniation, there might be complications related to liver function.
2. Gastroschisis:
- Intestinal Damage: Prolonged exposure of the intestines to the amniotic fluid can cause them to become thickened, shortened, or even necrotic (dead).
- Infection: The exposed intestines are at a higher risk of getting infections.
- Bowel Atresia: The intestines might develop blockages or fail to develop a part of the intestinal lumen, leading to atresia.
- Bowel Obstruction: Similar to omphalocele, the exposed bowel loops in gastroschisis can become twisted or compressed.
- Feeding Challenges: Affected babies often face challenges related to feeding, which might require prolonged parenteral (IV) nutrition.
- Growth and Nutritional Issues: Due to feeding and absorption challenges, there might be growth and nutritional concerns.
- Loss of Fluid: Since the intestines are outside the body, there might be increased fluid loss, leading to dehydration or electrolyte imbalances.
- Delayed Bowel Function: It may take longer for the intestines to start functioning normally after they are surgically placed back into the abdomen.
For both conditions, early detection, prompt surgical intervention (when indicated), and careful postoperative care are vital in minimizing these complications and ensuring the best possible outcomes for the affected newborns.
Diagnosis and Detection of Omphalocele and Gastroschisis
Diagnosing and detecting Omphalocele and Gastroschisis are of utmost importance, as early detection can guide management and improve outcomes for both the fetus and mother. Here’s how these conditions are typically diagnosed and detected:
1. Prenatal Ultrasound:
- Omphalocele:
- On ultrasound, an omphalocele appears as a central anterior abdominal wall defect containing herniated abdominal organs, covered by a membrane.
- Larger omphaloceles can be diagnosed as early as the first trimester, while smaller ones are typically seen in the second trimester.
- The presence of associated anomalies, especially cardiac, can also be assessed via detailed ultrasound.
- Gastroschisis:
- Gastroschisis is often diagnosed during the second trimester ultrasound as an abdominal wall defect, usually to the right of the umbilicus, with herniated bowel loops floating freely in the amniotic fluid without a covering sac.
- Due to the free-floating intestines, there’s often increased bowel motility observed on ultrasound.
- Serial ultrasounds may be done to monitor bowel appearance for signs of bowel damage, such as dilatation or thickening.
2. Maternal Serum Alpha-Fetoprotein (MSAFP) Screening:
- Both conditions can be associated with elevated levels of alpha-fetoprotein in the mother’s blood, especially gastroschisis.
3. Fetal MRI (Magnetic Resonance Imaging):
- While ultrasound is the primary mode of diagnosis, an MRI can be useful in selected cases to further evaluate the extent of the defect, especially in cases where ultrasound findings are equivocal or where there’s a suspicion of additional abnormalities.
4. Genetic Testing and Counseling:
- Omphalocele:
- Since it’s often associated with chromosomal abnormalities, amniocentesis might be offered to check for genetic issues.
- Parents might be referred for genetic counseling to understand the potential implications and risks associated with chromosomal anomalies.
- Gastroschisis:
- Genetic testing is not typically pursued for isolated gastroschisis, as it is rarely associated with chromosomal abnormalities.
5. Physical Examination Post-Birth:
- In cases where the conditions weren’t diagnosed prenatally, both omphalocele and gastroschisis are evident upon a physical examination at birth due to the visible abdominal wall defects.
Early detection not only allows for informed decisions regarding the pregnancy but also aids in planning delivery in a tertiary care center with the necessary neonatal and surgical facilities for immediate intervention post-birth.
Treatment and Management for Omphalocele and Gastroschisis
Treatment and management of both Omphalocele and Gastroschisis require specialized care, often involving a multidisciplinary team approach that includes obstetricians, neonatologists, pediatric surgeons, and other specialized medical staff. Here’s how each condition is typically treated and managed:
1. Omphalocele:
- Prenatal Care: Monitoring the size of the omphalocele and checking for associated anomalies through routine ultrasounds. In cases of significant associated anomalies, genetic counseling may be provided.
- Birth Planning: Consideration for delivery at a tertiary care center with specialized neonatal and surgical facilities. A Cesarean section might be recommended in large omphaloceles to prevent trauma during delivery.
- Post-birth Management:
- Small Omphaloceles: Surgical closure shortly after birth, where the sac is removed and the abdominal wall is sutured.
- Large Omphaloceles: Immediate surgery might not always be possible. The sac might be initially covered with a sterile dressing (often referred to as a “paint and wait” approach). Gradual reduction of the contents back into the abdominal cavity over days to weeks may be performed before final surgical closure. This is to avoid tension on the abdominal wall and allow for abdominal capacity to accommodate the organs.
- Associated Anomalies: These will need appropriate evaluation and management. For instance, cardiac defects might require pediatric cardiology consultations and potential interventions.
2. Gastroschisis:
- Prenatal Care: Regular ultrasounds to monitor the bowel’s appearance for signs of damage or complications.
- Birth Planning: Delivery in a tertiary care center is essential, preferably before the onset of labor to avoid prolonged rupture of membranes and potential bowel exposure.
- Immediate Post-birth Management:
- Protecting the exposed bowel by placing them in a sterile plastic pouch (often referred to as a “silo”) to reduce heat and fluid loss.
- The baby is often intubated to protect the airway and to prevent the baby from swallowing air, which can inflate the stomach and further compromise the return of the bowel.
- IV fluids, antibiotics, and sometimes vasopressor medications to support blood pressure.
- Surgical Management:
- Primary Closure: If feasible, the surgeon will reposition the intestines inside the abdomen and close the defect soon after birth.
- Staged Reduction: If primary closure isn’t possible due to the swelling of the intestines or the size of the defect, the intestines are gradually pushed back into the abdomen over days using the silo. Once inside, the defect can be closed either surgically or using a special adhesive.
- Postoperative Care:
- Monitoring for complications like infection, bowel obstruction, or necrotizing enterocolitis (NEC).
- Slow introduction of feeds while ensuring the intestines are functioning well. The baby might initially be on total parenteral nutrition (TPN) until bowel function normalizes.
Both conditions often require a prolonged stay in the neonatal intensive care unit (NICU). It’s essential for families to receive support, counseling, and education throughout the process, from diagnosis to treatment and post-operative care.
Prognosis of Omphalocele and Gastroschisis
The prognosis for both Omphalocele and Gastroschisis largely depends on the severity of the defect, the presence of associated anomalies, and the timeliness and effectiveness of medical and surgical intervention. Here’s a general outlook for each condition:
1. Omphalocele:
- Isolated Omphalocele: If the defect is small and there are no associated anomalies, the prognosis is generally good with appropriate surgical treatment.
- Large Omphalocele: Babies with a large omphalocele may require prolonged hospital stays and multiple surgeries, but many can eventually lead normal lives with appropriate management.
- Associated Anomalies: The prognosis can be more guarded when there are other congenital anomalies, especially cardiac defects or chromosomal abnormalities. For example, conditions like Trisomy 18, often associated with omphalocele, have a poor prognosis.
- Long-Term Outlook: Some children might have long-term feeding and growth challenges, and there can be potential cosmetic concerns related to the surgical repair, which might necessitate further surgical interventions in the future.
2. Gastroschisis:
- Isolated Gastroschisis: Most babies with gastroschisis, when managed promptly and effectively, have a good prognosis. They typically lead healthy lives after initial hospitalization and surgical intervention.
- Bowel Damage: If there is significant bowel damage or complications like necrotizing enterocolitis (NEC), the prognosis can be more challenging. Such babies might face long-term nutritional and digestive issues.
- Long-Term Outlook: While most children recover well, some might have long-term complications related to digestion and nutrition, bowel motility issues, or potential cosmetic concerns related to the surgical repair.
For both conditions, early detection and a comprehensive, multidisciplinary approach to treatment and management play a crucial role in optimizing outcomes. With advances in prenatal care, neonatal intensive care, and pediatric surgery, the prognosis for both omphalocele and gastroschisis has significantly improved over the years.
Conclusion
Omphalocele and Gastroschisis are congenital abdominal wall defects that present distinct clinical features, requiring specialized care and intervention. While Omphalocele is characterized by the herniation of abdominal organs within a protective sac, Gastroschisis involves exposed intestines without any sac covering. Early detection through prenatal screening, coupled with prompt surgical intervention post-birth, is crucial for optimizing outcomes.
While both conditions may pose challenges, advances in neonatal and surgical care have led to improved prognoses. As each case is unique, individualized treatment and a multidisciplinary approach are paramount to ensuring the best possible outcome for affected newborns.