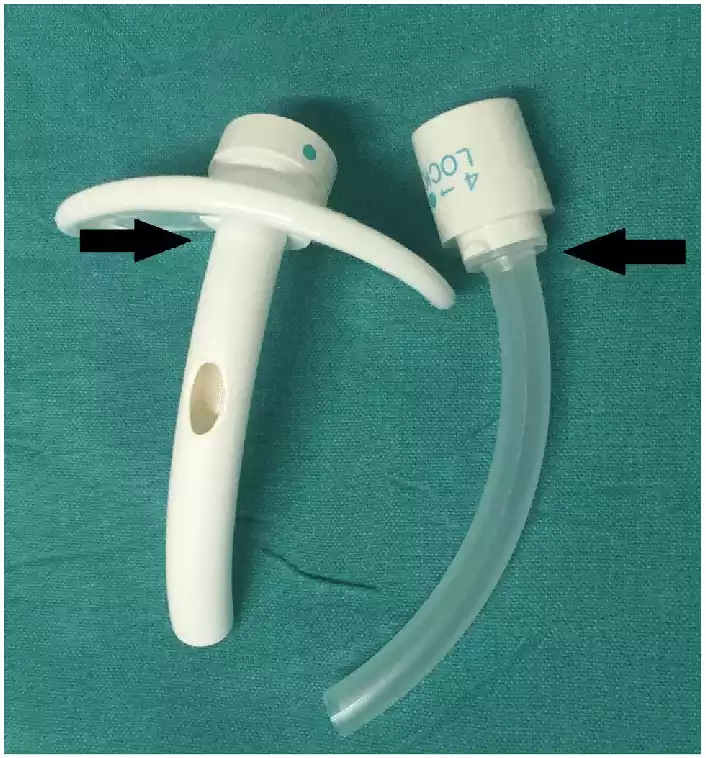
Fenestrated and Non-fenestrated Tracheostomy Tube: A Tracheostomy Tube is a medical device inserted into a surgically created opening in the trachea (windpipe) to maintain an open airway. These tubes come in various types, each tailored to specific clinical needs. Two primary types are the fenestrated and non-fenestrated tracheostomy tubes. A Fenestrated Tracheostomy Tube features one or more holes (fenestrations) along its cannula, allowing for functions such as facilitated speech and assisted breathing through the upper airway.
A Non-Fenestrated Tracheostomy Tube lacks these fenestrations, providing a continuous and unobstructed airway passage. This design is especially beneficial for patients on mechanical ventilation or those at risk of aspiration. The choice between these tubes is contingent upon the patient’s clinical status and specific therapeutic objectives.
Fenestrated Tracheostomy Tube
A Fenestrated Tracheostomy Tube is a specific type of tracheostomy tube designed with one or more holes (fenestrations) along the length or curvature of its outer and/or inner cannula.

These fenestrations serve multiple purposes:
- Breathing through the Upper Airway: The fenestrations allow the patient to breathe through their upper airway (including the larynx, or voice box) when the tracheostomy tube’s inner cannula is removed or when it’s also fenestrated and aligned with the fenestrations of the outer cannula.
- Speech: One of the significant benefits of the fenestrated tracheostomy tube is that it can enable speech. By allowing air to pass through the vocal cords when the patient exhales (and often in combination with a speaking valve or capping the tracheostomy tube), the patient can produce sound and speak.
- Weaning from the Tracheostomy: The fenestrated tracheostomy tube can be instrumental in the process of weaning a patient off the tracheostomy tube. By allowing them to breathe partially or wholly through their upper airway, it can facilitate a smoother transition to normal respiratory function.
However, it’s essential to understand that not every patient is a candidate for a fenestrated tracheostomy tube. Patients at risk for aspiration or those with excessive secretions might not be suitable candidates due to the risk of these secretions entering the fenestrations and causing complications. Proper care and assessment are required when using a fenestrated tube.
Advantages of Fenestrated Tracheostomy Tube
Fenestrated tracheostomy tubes offer several advantages over their non-fenestrated counterparts under appropriate conditions. Here are some of the primary advantages of fenestrated tracheostomy tubes:
- Facilitated Speech:
- Fenestrated tubes allow air to pass through the fenestrations and then over the vocal cords when the patient exhales.
- With proper cuff management (if the tube has a cuff) and alignment of the fenestrations, patients can produce sound and speak.
- Airway Humidification:
- The fenestrations permit some airflow through the patient’s upper airway, which can aid in humidifying and warming the inhaled air more naturally.
- Improved Swallowing:
- Some patients may find swallowing easier with a fenestrated tube since it allows for better coordination between breathing and swallowing.
- Enhanced Sensation:
- The fenestrations can restore some level of airflow through the patient’s natural airway, potentially improving the sensation in the throat and reducing the foreign body feeling associated with a tracheostomy.
- Facilitation of Weaning:
- Fenestrated tubes can be used in the process of weaning a patient from the tracheostomy.
- They enable the patient to breathe increasingly through their upper airway, preparing the lungs and muscles for natural breathing and potentially leading to decannulation (removal of the tracheostomy tube).
- Psychological Benefits:
- Being able to speak can have significant psychological benefits for patients, as communication is a fundamental human need.
- This can also improve patient-staff and patient-family interactions, positively impacting the overall care and recovery process.
- Enhanced Cough Reflex:
- The fenestrations allow for a more robust cough reflex since some air is directed up through the larynx, facilitating better secretion clearance.
- Respiratory Training:
- The resistance from the fenestrations can assist in strengthening the respiratory muscles when the patient breathes through them.
It’s essential to understand, that while fenestrated tracheostomy tubes offer these advantages, they might not be suitable for all patients. The potential benefits should be weighed against the risks, and the decision to use a fenestrated tube should be made based on individual patient needs and clinical assessment.
Non-fenestrated Tracheostomy Tube
A Non-Fenestrated Tracheostomy Tube is a type of tracheostomy tube that lacks fenestrations or holes along its cannula. In other words, the tube is solid throughout its length without any openings aside from its primary lumen, which is intended to provide an airway for the patient.

The non-fenestrated tracheostomy tube serves several key functions:
- Secure Airway: It provides a continuous and unobstructed pathway for air, making it ideal for patients who require stable and secure respiratory support, especially those on mechanical ventilation.
- Airway Protection: Without fenestrations, there is a reduced risk of aspiration, which makes the non-fenestrated tube suitable for patients at risk of aspirating oral or gastric contents into the lungs.
- Secretion Management: Patients with heavy secretions can benefit from a non-fenestrated tube since there’s no risk of the secretions entering or blocking fenestrations. This ensures that the primary lumen remains clear for air passage.
Non-Fenestrated tracheostomy tubes is that they generally do not allow for speech unless specific maneuvers, such as temporary capping or using speaking valves, are employed. This is because air doesn’t naturally pass over the vocal cords with a non-fenestrated tube in place.
Advantages of Non-fenestrated Tracheostomy Tube
Non-fenestrated tracheostomy tubes, while lacking the fenestrations present in their counterparts, provide several unique advantages in specific clinical scenarios. Here are the primary advantages of non-fenestrated tracheostomy tubes:
- Secure Airway:
- Non-fenestrated tubes offer a continuous and unobstructed pathway for air, making them ideal for patients who require a stable and uncompromised respiratory passage.
- Reduced Risk of Aspiration:
- Without fenestrations, there’s a reduced likelihood of oral or gastric contents being aspirated into the trachea and lungs. This makes them ideal for patients at risk of aspiration.
- Effective for Mechanical Ventilation:
- Patients on mechanical ventilation often use non-fenestrated tubes to ensure a consistent and secure airway, free from potential air leaks through fenestrations.
- Less Maintenance in Heavy Secretions:
- For patients with heavy secretions, non-fenestrated tubes can be beneficial as there’s no risk of these secretions entering or clogging fenestrations.
- Airway Protection:
- Non-fenestrated tubes provide a more secure barrier between the lower airway and external environment, which can be especially important in patients with compromised immunity or heightened risk of infections.
- Consistent Positive Pressure:
- If a patient requires positive pressure ventilation, non-fenestrated tubes ensure that the pressure is consistently maintained, as there are no fenestrations for potential air leaks.
- Reduced Risk of Granulation Tissue:
- Fenestrations in tracheostomy tubes can sometimes lead to the formation of granulation tissue, which can cause obstructions or complications. Non-fenestrated tubes do not present this specific risk related to fenestrations.
- General Versatility:
- Non-fenestrated tracheostomy tubes are versatile and can be used across a broader range of patients and conditions, especially when there’s uncertainty about a patient’s risk factors or when long-term tracheostomy is anticipated.
It’s essential to understand that while non-fenestrated tracheostomy tubes offer these advantages, they also come with limitations, such as reduced natural airway function and limited speech capabilities. The decision to use a non-fenestrated tube should always be based on a comprehensive clinical assessment and the specific needs of the individual patient.
Comparison table of Fenestrated and Non-fenestrated Tracheostomy Tube
Below is a comparison table outlining the differences between fenestrated and non-fenestrated tracheostomy tubes:
| Feature/Function | Fenestrated Tracheostomy Tube | Non-fenestrated Tracheostomy Tube |
|---|---|---|
| Definition | Tube with one or more holes (fenestrations) along its cannula. | Tube without any fenestrations along its cannula. |
| Breathing through Upper Airway | Allows for breathing through the upper airway when inner cannula is removed or aligned. | Does not allow for breathing through the upper airway in the same manner. |
| Speech | Facilitates speech by allowing air to pass through vocal cords. | Typically does not allow for speech unless combined with certain techniques or devices. |
| Risk of Aspiration | Higher risk due to the presence of fenestrations. | Reduced risk because of the absence of fenestrations. |
| Airway Protection | Less secure due to fenestrations; not ideal for patients at high risk of aspiration. | Offers more secure airway protection, suitable for patients at risk of aspiration. |
| Secretion Management | Risk of secretions entering or blocking fenestrations. | No risk of secretions blocking fenestrations as there aren’t any; may require more frequent suctioning. |
| Weaning from Tracheostomy | Often used in the weaning process as it allows for gradual transition to normal respiratory function. | Not typically used for weaning in the same manner as the fenestrated tube. |
| Use with Mechanical Ventilation | Can be used, but care must be taken to ensure the fenestrations are sealed if a cuffed tube is used. | Commonly used for patients on mechanical ventilation. |
This table provides a summarized comparison, and the choice between the two types will often depend on the specific clinical needs and condition of the patient.
Similarities between Fenestrated and Non-fenestrated Tracheostomy Tube
While fenestrated and non-fenestrated tracheostomy tubes serve somewhat different purposes and have distinct features, they also share several similarities, given their fundamental role as tracheostomy tubes.
Here’s a list of their shared characteristics:
Similarities Between Fenestrated and Non-fenestrated Tracheostomy Tube:
- Purpose: Both types are designed to maintain an open airway by being inserted into the trachea through a surgical opening in the neck.
- Structure: Both typically have an outer cannula that stays in place in the trachea and an inner cannula that can be removed and cleaned.
- Material Composition: Both types can be made of similar materials, such as PVC (polyvinyl chloride), silicone, or metal.
- Cuff Availability: Both fenestrated and non-fenestrated tubes can come with or without a cuff. The cuff, when inflated, seals the trachea to prevent aspiration and allows for positive pressure ventilation.
- Securement: Both types of tubes are typically secured in place using tracheostomy ties or holders to prevent accidental dislodgement.
- Cleaning and Maintenance: Both tubes require regular care, including cleaning and suctioning, to ensure they remain patent and free from secretions.
- Replacement Schedule: Both types will typically have a recommended replacement or rotation schedule to ensure patient safety and maintain tube integrity.
- Potential Complications: Both types can lead to similar complications if not properly managed, such as infection, tracheal injury, granulation tissue formation, and tube blockage or dislodgment.
- Decannulation: Both tubes can be eventually removed, or “decannulated,” once the patient’s airway is stable and they no longer need it, though the process and criteria might differ.
- Application: Both types can be utilized in various healthcare settings, from intensive care units to home care, depending on the patient’s clinical requirements.
Understanding both the similarities and differences between fenestrated and non-fenestrated tracheostomy tubes is essential for healthcare providers to ensure the appropriate selection and management of the tracheostomy tube based on a patient’s individual needs.
Choosing the Right Tube for the Patient
Choosing the right tracheostomy tube for a patient is a critical decision that can greatly impact their comfort, safety, and overall clinical outcome. This choice should be based on a comprehensive evaluation of the patient’s clinical condition and the specific needs and goals of tracheostomy care. Here’s a guide on how to choose the right tube:
- Assess Clinical Indication:
- Mechanical Ventilation: If a patient requires long-term mechanical ventilation, a non-fenestrated tube might be more suitable due to its secure and continuous airway pathway.
- Risk of Aspiration: For patients with a high risk of aspirating oral or gastric contents, a non-fenestrated tube is often recommended.
- Speech and Swallowing Goals: If one of the primary objectives is to allow the patient to speak or improve swallowing, a fenestrated tube might be beneficial.
- Evaluate Patient’s Anatomy:
- Consider the size and shape of the patient’s neck and trachea. Tubes come in various lengths, curvatures, and diameters, so selecting a tube that fits the patient’s anatomy is crucial to avoid complications.
- Determine Need for Cuff:
- If the patient needs positive pressure ventilation or is at risk of aspiration, a cuffed tube might be required.
- If the primary goal is to allow speech or if the patient is at low risk for aspiration, a cuffless tube might be appropriate.
- Assess Secretion Levels:
- If a patient has heavy secretions, a non-fenestrated tube might be more manageable as there’s no risk of secretions entering or clogging the fenestrations.
- Evaluate Weaning Potential:
- For patients on the path to being weaned off the tracheostomy, a fenestrated tube can be helpful as it allows for a smoother transition to natural respiratory function.
- Consider Long-Term vs. Short-Term Use:
- Some tubes are designed for short-term use (like certain cuffed tubes used in ICU settings), while others are more suited for long-term placement.
- Evaluate Patient Comfort:
- Some patients might find certain tubes more comfortable than others. For example, a tube made of soft silicone might be more comfortable for long-term use than one made of a harder material.
- Safety and Emergency Concerns:
- Always have an emergency tracheostomy tube kit available that contains a tube of the same size and one size smaller than the patient’s current tube. This is critical in case of accidental decannulation or blockage.
- Regular Re-Evaluation:
- As the patient’s condition evolves, the type of tracheostomy tube they require might change. Regular assessment by healthcare professionals can ensure the tube remains appropriate for their needs.
- Involve a Multidisciplinary Team:
- Involving a team that includes respiratory therapists, otolaryngologists, intensivists, speech therapists, and nursing staff can provide a comprehensive perspective on the best tube choice.
The choice of tracheostomy tube should prioritize patient safety and comfort while aligning with the therapeutic goals. This decision should be revisited regularly to ensure the selected tube remains optimal for the patient’s evolving needs.
Risks and Precautions
Both fenestrated and non-fenestrated tracheostomy tubes present their own set of risks. Understanding these risks and taking appropriate precautions is vital for ensuring patient safety and optimizing clinical outcomes.
Fenestrated Tracheostomy Tube
Risks:
- Aspiration Risk: The fenestrations can allow oral or gastric contents to enter the trachea, potentially leading to aspiration pneumonia.
- Granulation Tissue: The presence of fenestrations can cause granulation tissue to form, which can obstruct the airway or create a source of bleeding.
- Misalignment: Fenestrations can become misaligned, leading to impaired airflow or inability to pass suction catheters or other instruments.
- Secretion Blockage: Secretions can block the fenestrations, impacting the tube’s effectiveness and potentially obstructing the airway.
- Decreased Positive Pressure: During mechanical ventilation, fenestrations can cause a decrease in positive pressure unless sealed properly.
Precautions:
- Regular Assessment: Monitor for signs of aspiration and regularly assess lung sounds.
- Proper Tube Placement: Ensure that the fenestrations are correctly aligned.
- Cuff Management: If the tube has a cuff, manage it appropriately to prevent aspiration, especially during speaking or swallowing.
- Routine Cleaning: Clean the tube regularly to ensure that secretions do not block the fenestrations.
Non-fenestrated Tracheostomy Tube
Risks:
- Impaired Speech: Without fenestrations, it’s more challenging for the patient to speak.
- Impaired Swallowing: The continuous tube can interfere with the natural swallowing process.
- Risk of Tube Obstruction: Accumulated secretions, mucous plugs, or blood can obstruct the tube.
- Tracheal Injury: Prolonged use can potentially lead to tracheal injury or the formation of tracheal stenosis.
Precautions:
- Regular Suctioning: Due to the risk of tube obstruction, regular suctioning is necessary to maintain a clear airway.
- Speech and Swallowing Therapy: Engage speech and swallowing therapists to assist the patient with communication and swallowing techniques.
- Routine Tube Care: Regular cleaning and care can prevent potential complications.
- Monitor for Complications: Regularly assess for signs of tracheal injury, granulation tissue formation, or other complications.
For both types of tubes:
- Always have an emergency tracheostomy kit available.
- Regularly assess the stoma site for signs of infection or skin breakdown.
- Monitor the patient’s overall respiratory status, including oxygen saturation, breathing patterns, and comfort.
Ensuring that the healthcare team is well-trained in tracheostomy care and understands the unique risks and precautions associated with each type of tube is crucial.
Cleaning and Maintenance
Cleaning and maintaining both fenestrated and non-fenestrated tracheostomy tubes are essential for preventing infections, ensuring patient comfort, and promoting optimal airflow. While the fundamental cleaning and maintenance steps are similar for both types, there are specific considerations to take into account due to the fenestrations in the former. Here’s a guide:
General Steps for Both Types
- Daily Cleaning:
- Supplies: Clean gloves, normal saline or hydrogen peroxide, soft cloth or gauze, soft-bristle brush or pipe cleaners, sterile water, clean basin or bowl, clean towel, and sterile lubricant (if needed).
- Remove and soak the inner cannula (if present and disposable) in the solution.
- Gently scrub the cannula using the brush or pipe cleaners.
- Rinse thoroughly, especially if hydrogen peroxide was used.
- Allow it to air dry and then reinsert.
- Stoma Care:
- Clean the stoma site daily or when soiled using mild soap and water.
- Inspect for signs of infections or irritations.
- Humidification:
- Ensure proper humidification as tracheostomy bypasses the natural humidification process of the upper airway.
- Regular Suctioning:
- Suction the tube to remove mucus and secretions, preventing blockages.
Specific for Fenestrated Tracheostomy Tubes
- Careful Cleaning:
- Ensure fenestrations are free from mucus or debris. Blockages here can interfere with the intended functions like speaking or breathing through the upper airway.
- Cuff Management (if the tube has a cuff):
- When deflated for speaking or swallowing, ensure no secretions enter the fenestrations, which could lead to aspiration.
- Regular Inspection:
- Check the integrity of the fenestrations over time. Repeated cleaning might enlarge them or cause wear and tear.
Specific for Non-fenestrated Tracheostomy Tubes
- Thorough Cleaning:
- As these tubes don’t have fenestrations, ensure the main lumen is free from any mucus or obstructions for optimal airflow.
- Cuff Management (if the tube has a cuff):
- Regularly check the cuff for any leaks and ensure it maintains proper inflation.
- Regular Inspection:
- Look for any structural damage or wear that might compromise its continuous airway pathway.
Maintenance for Both
- Replace Dressings: Change tracheostomy dressings as needed to keep the area dry and clean.
- Tube Change: Depending on the type and patient’s condition, tubes might need periodic changing.
- Emergency Kit: Always have an emergency tracheostomy kit available in case of accidental decannulation or blockages.
Whether a tracheostomy tube is fenestrated or non-fenestrated, a regular and meticulous cleaning and maintenance routine is crucial. Such attention ensures longevity of the tube, patient safety, and optimal therapeutic benefits.
Final Thoughts
Fenestrated and Non-Fenestrated Tracheostomy tubes serve as vital tools in respiratory care, each designed to address specific clinical needs. Fenestrated tubes, with their characteristic holes, offer enhanced functionalities like facilitated speech and breathing through the upper airway, while non-fenestrated tubes provide a continuous, unobstructed pathway, ideal for mechanical ventilation and those at risk of aspiration.
The choice between them hinges on a thorough evaluation of the patient’s medical condition and the desired therapeutic outcomes. Whichever tube is selected, diligent care, cleaning, and maintenance are paramount to ensure patient safety, comfort, and the prevention of potential complications.