Neoplastic and Non-neoplastic Polyps are growths that can be found in various mucosal linings, most commonly the gastrointestinal tract. Neoplastic polyps, such as adenomas, harbor cellular abnormalities and carry a potential risk of progressing to cancer. On the other hand, non-neoplastic polyps, like hyperplastic or inflammatory polyps, are typically benign and lack malignant potential. Despite their differences, both types underscore the importance of regular medical screenings, as early detection and appropriate management can prevent potential complications and improve health outcomes.
What are Neoplastic Polyps?
Neoplastic polyps are abnormal growths that arise from the mucosal lining of an organ, characterized by dysplasia, or abnormal cell maturation. These polyps possess the potential to progress to cancer over time. Histologically, neoplastic polyps demonstrate cellular atypia and can be further classified into various subtypes, including adenomas in the colon.
The risk of progression to malignancy depends on several features, such as size, histological type, degree of dysplasia, and the presence of certain architectural patterns. Identifying and removing neoplastic polyps, particularly in the colon, is a primary strategy for preventing the development of certain cancers.
Characteristics of Neoplastic Polyps
Neoplastic polyps exhibit specific characteristics, which hint at their potential for malignant transformation. Here are some of the defining features and characteristics of neoplastic polyps:
- Cellular Dysplasia: At the cellular level, neoplastic polyps display dysplasia, which involves abnormalities in cell maturation and architecture. This dysplasia can range from mild to severe.
- Histological Types: The most common type of neoplastic polyp in the colon is the adenoma. Adenomas can be further classified based on their growth pattern and histology into tubular adenomas, villous adenomas, and tubulovillous adenomas.
- Growth Pattern: Neoplastic polyps can exhibit different growth patterns. Some may grow in a sessile fashion (flat or broad-based) while others may have a pedunculated appearance (stalk-like growth).
- Potential for Malignancy: Not all neoplastic polyps will turn into cancer, but they have the inherent potential. The risk of malignant transformation increases with the size of the polyp, the degree of dysplasia, and certain histological features (e.g., a predominance of villous architecture).
- Size: Larger polyps generally carry a higher risk of malignant transformation. Polyps larger than 1 cm are of particular concern.
- Molecular Changes: Various genetic and epigenetic changes can be observed in neoplastic polyps, which can influence their progression to malignancy. For example, mutations in the APC gene are commonly seen in colorectal adenomas.
- Location: Neoplastic polyps can occur in various parts of the body, with the colon being a common site. However, they can also be found in the stomach, esophagus, small intestine, and other locations.
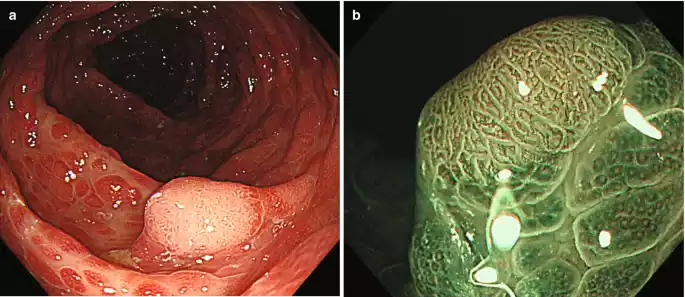
- Appearance: Endoscopically, neoplastic polyps may have a distinct appearance compared to non-neoplastic polyps. They can be redder, more irregular, and may bleed easily upon contact.
Early detection and removal of neoplastic polyps, especially in the colon, are crucial to prevent progression to cancer. Regular screenings, like colonoscopies, are recommended for at-risk populations to identify and excise these lesions.
Types of Neoplastic Polyps
Neoplastic polyps have the potential to progress to cancer and are characterized by cellular dysplasia. Several types of neoplastic polyps exist, particularly within the gastrointestinal (GI) tract. Here are the primary types:
- Adenomas: These are the most common type of neoplastic polyps found in the colon. They can be further classified based on their architecture and histology:
- Tubular Adenomas: Composed predominantly of tubular structures. They are the most common type and have a lower risk of malignancy compared to villous adenomas.
- Villous Adenomas: Characterized by long, finger-like projections. They have a higher risk of malignancy.
- Tubulovillous Adenomas: A mix of both tubular and villous architectures. Their risk of malignant transformation is intermediate between tubular and villous adenomas.
- Serrated Polyps: A heterogeneous group of polyps that can be neoplastic or non-neoplastic. The neoplastic ones include:
- Sessile Serrated Adenomas/Polyps (SSA/P): These have the potential to become cancerous and follow a different molecular pathway than traditional adenomas.
- Traditional Serrated Adenomas (TSA): Less common than SSA/Ps but have a clear neoplastic potential.
- Intramucosal Carcinoma: Represents early cancer that is confined to the mucosal layer of the GI tract. It has not yet invaded the deeper layers or metastasized but is a definite malignant change from a polyp.
- Hamartomatous Polyps: While primarily non-neoplastic, in the context of certain syndromes, these polyps may carry a risk for malignancy. For example:
- Peutz-Jeghers Polyps: Found in the Peutz-Jeghers syndrome, these hamartomatous polyps primarily occur in the small intestine. Patients with this syndrome have an increased risk of various cancers.
- Adenomatous Polyps of the Stomach: Less common than colonic adenomas but still possess a risk for malignant transformation.
Outside of the GI tract, the term “neoplastic polyps” might be used more broadly in other organs to describe growths with malignant potential, but the context and specifics would vary depending on the organ and tissue type.
What are Non-neoplastic Polyps?
Non-neoplastic polyps are abnormal growths that arise from the mucosal lining of an organ, but unlike neoplastic polyps, they do not have the inherent potential to progress to cancer. These polyps are typically benign and result from various causes, including inflammation, hyperplasia, or other non-malignant cellular changes. Common types of non-neoplastic polyps include hyperplastic polyps, hamartomatous polyps, and inflammatory polyps.
Their presence is often incidental, and they generally do not pose a significant risk of malignancy. However, it’s important to accurately diagnose them to differentiate from their neoplastic counterparts and guide appropriate management.
Characteristics of Non-neoplastic Polyps
Non-neoplastic polyps are benign growths that arise from the mucosal lining of an organ and do not have the inherent potential to progress to cancer. Their characteristics differ significantly from neoplastic polyps:
- Cellular Architecture: Unlike neoplastic polyps, non-neoplastic polyps do not show dysplasia. The cells maintain their normal architecture and maturation pattern, although they may proliferate excessively.
- Histological Types:
- Hyperplastic Polyps: Common in the colon, these are small mucosal proliferations without the risk of malignant transformation.
- Hamartomatous Polyps: Resulting from an overgrowth of normally organized tissue, examples include Peutz-Jeghers and juvenile polyps.
- Inflammatory Polyps: These arise secondary to chronic inflammation, often seen in conditions like inflammatory bowel disease.
- Growth Pattern: Typically, non-neoplastic polyps grow without the irregularities seen in neoplastic ones. Their growth is more uniform.
- Lack of Malignant Potential: By definition, non-neoplastic polyps don’t have the potential to evolve into malignancies. However, their presence might signal other underlying conditions, especially inflammatory or genetic syndromes, that may carry other risks.
- Size and Appearance: Many non-neoplastic polyps, especially hyperplastic ones, are small and pale. However, size and appearance can vary depending on the type and location of the polyp.
- Location: While they can occur throughout the gastrointestinal tract, certain non-neoplastic polyps have preferred locations. For example, hyperplastic polyps are often found in the colon, whereas hamartomatous polyps may be seen throughout the gastrointestinal tract in syndromic conditions.
- Molecular and Genetic Features: Some non-neoplastic polyps, especially hamartomatous ones associated with genetic syndromes, can exhibit particular genetic patterns. For example, mutations in the STK11 gene are linked with Peutz-Jeghers syndrome.
- Associated Conditions: The presence of certain non-neoplastic polyps may indicate other underlying conditions. For instance, inflammatory polyps are often seen in the context of inflammatory bowel disease.
While non-neoplastic polyps generally don’t pose a malignancy risk, it’s crucial to accurately diagnose them. This ensures appropriate patient management, especially if they signal other underlying conditions or syndromes.
Types of Non-neoplastic Polyps
Non-neoplastic polyps are growths that do not possess the cellular abnormalities seen in neoplastic polyps and typically do not have the potential to progress to cancer. Here are some of the main types of non-neoplastic polyps:
- Hyperplastic Polyps:
- Most common type of non-neoplastic polyp.
- Typically small and found in the rectum or sigmoid colon.
- Generally have no potential to become cancerous, though there’s ongoing discussion about certain large or serrated hyperplastic polyps in the proximal colon.
- Inflammatory Polyps (Pseudopolyps):
- Result from chronic inflammation, often in the setting of inflammatory bowel disease (IBD), such as ulcerative colitis or Crohn’s disease.
- They are not true polyps but rather are areas of regenerating colonic mucosa surrounded by areas of ulceration or inflammation.
- Hamartomatous Polyps:
- Result from an overgrowth of normal tissue components of the mucosa.
- Can occur sporadically or as part of inherited syndromes such as:
- Peutz-Jeghers Syndrome: Polyps throughout the gastrointestinal tract, often with mucocutaneous pigmentation.
- Juvenile Polyposis: Multiple hamartomatous polyps in the colon, stomach, and small intestine.
- Cronkhite-Canada Syndrome: Hamartomatous polyps in the stomach and intestines, often with skin, hair, and nail changes.
- Lymphoid Polyps:
- Composed of lymphoid tissue.
- Typically found in children and are usually located in the rectum.
- Mucosal and Submucosal Polyps:
- Often related to conditions where there is an overproduction of mucus, such as cystic fibrosis.
These polyps are typically benign in nature and do not have the same risk of progression to malignancy as neoplastic polyps. Their management may vary based on the type, size, and location of the polyp, as well as the presence of any associated syndromes or conditions.
Comparison table of Neoplastic and Non-neoplastic Polyps
Here’s a simplified comparison table of neoplastic and non-neoplastic polyps based on various parameters:
| Feature | Neoplastic Polyps | Non-neoplastic Polyps |
|---|---|---|
| Cellular Characteristics | Display dysplasia (abnormal cell maturation) | Maintain normal cell architecture |
| Malignant Potential | Have potential to progress to cancer | Typically lack malignant potential |
| Common Examples | Adenomas (tubular, villous, tubulovillous), Serrated polyps (SSA/P, TSA) | Hyperplastic polyps, Hamartomatous polyps (e.g., Juvenile), Inflammatory polyps |
| Appearance | Can be varied, but may show irregularities; might be redder or bleed easily | Often uniform in appearance; can be small and pale |
| Associated Genetic Changes | Often have mutations or other molecular changes (e.g., APC gene mutations in colorectal adenomas) | Fewer specific genetic associations; some syndromic conditions like Peutz-Jeghers have genetic basis |
| Risk Factors | Age, family history, certain genetic syndromes | Varies; can be related to inflammation, genetic syndromes, or idiopathic |
| Management | Often require removal and surveillance due to cancer risk | Management depends on type, size, and location; many don’t require aggressive treatment |
| Location | Commonly in the colon but can occur throughout the GI tract and other organs | Commonly in the colon but can be seen throughout the GI tract and other areas |
This table provides a general overview, but the specifics can vary based on the exact type and location of the polyp, the patient’s clinical context, and advances in medical knowledge. Always consult relevant clinical guidelines and literature when making decisions related to polyp management.
Diagnosis & Treatment of Neoplastic and Non-neoplastic Polyps
The diagnosis and treatment approaches for both neoplastic and non-neoplastic polyps have similarities, but specific management can vary based on the nature of the polyp.
Diagnosis
Both Neoplastic and Non-neoplastic Polyps
- Endoscopy:
- Colonoscopy: A primary method for detecting polyps in the colon.
- Sigmoidoscopy: Examines only the left side of the colon.
- Upper Endoscopy (EGD): For the esophagus, stomach, and duodenum.
- Imaging:
- CT Colonography (Virtual Colonoscopy): Uses CT scans for visualization.
- Barium Enema: An X-ray procedure of the colon and rectum.
- Histopathology:
- Biopsy: Polyps identified during endoscopy can be biopsied. The tissue is then histologically examined to distinguish between neoplastic and non-neoplastic.
Treatment
Neoplastic Polyps
- Endoscopic Removal:
- Polypectomy: Small neoplastic polyps can be removed during a colonoscopy.
- Endoscopic Mucosal Resection (EMR): Used for larger polyps.
- Endoscopic Submucosal Dissection (ESD): For even larger polyps or early-stage cancers.
- Surgery: If a polyp cannot be removed endoscopically or if there’s a concern about cancer spread, surgical removal might be needed.
- Regular Surveillance: Post-removal, regular check-ups are crucial to monitor for new polyps or potential malignancies.
Non-neoplastic Polyps
- Endoscopic Removal: Not all non-neoplastic polyps need to be removed, but if they’re causing symptoms or are of a significant size, they can be removed during an endoscopy.
- Observation: Many non-neoplastic polyps, like small hyperplastic polyps, don’t pose significant risks and might be monitored rather than removed.
- Treatment of Underlying Causes: For inflammatory polyps, treating the underlying inflammatory condition (e.g., ulcerative colitis) is essential.
- Regular Surveillance: If a person has conditions leading to multiple non-neoplastic polyps (e.g., certain syndromes), they might need regular check-ups.
Additional Notes:
- While treatments differ somewhat between neoplastic and non-neoplastic polyps, the mainstay of initial identification and management for both is endoscopy.
- It’s essential to accurately determine the nature of the polyp (biopsy and histology) as treatment, and follow-up recommendations can differ substantially.
- Genetic counseling and more frequent screenings might be recommended for individuals with family histories or genetic syndromes that predispose them to polyps or cancer.
- Communication between the patient and healthcare provider is vital. The treatment chosen often depends on the specific type, size, and location of the polyp, the patient’s overall health, and other factors.
Risk Factors & Prevention of Neoplastic and Non-neoplastic Polyps
The risk factors and prevention strategies for neoplastic and non-neoplastic polyps overlap in some areas but also have distinct differences.
Risk Factors
Neoplastic Polyps
- Age: Risk increases with age, especially after 50.
- Family History: Having close relatives with polyps or colorectal cancer increases the risk.
- Personal History: Having had polyps or colorectal cancer in the past.
- Inherited Syndromes: Such as familial adenomatous polyposis (FAP) or Lynch syndrome.
- Diet: High in red meat and low in fiber.
- Tobacco and Alcohol Use: Both are associated with an increased risk.
- Obesity: Being overweight increases the risk.
- Race: African Americans may have a higher risk of colorectal cancer.
- Type 2 Diabetes: Individuals with this condition have an increased risk.
Non-neoplastic Polyps
- Chronic Inflammation: Conditions like ulcerative colitis or Crohn’s disease can lead to inflammatory polyps.
- Age: Older individuals may have a higher chance of developing some non-neoplastic polyps.
- Diet and Lifestyle Factors: Similar to neoplastic polyps, certain dietary and lifestyle factors may play a role.
- Inherited Conditions: Syndromes like Peutz-Jeghers or juvenile polyposis can increase the risk.
Prevention
Neoplastic Polyps
- Regular Screening: Colonoscopies or other screening tests can identify and remove precancerous polyps.
- Dietary Changes: A diet high in fruits, vegetables, and whole grains, and low in red meat can reduce risk.
- Physical Activity: Regular exercise can reduce the risk of polyps and colorectal cancer.
- Avoiding Tobacco and Limiting Alcohol.
- Maintaining a Healthy Weight.
- Aspirin and NSAIDs: Some studies suggest they might reduce the risk, but they come with their own risks. Consultation with a physician is necessary.
- Calcium and Vitamin D Supplementation: May help in reducing the risk, but again, discuss with a doctor before starting any supplementation.
Non-neoplastic Polyps
- Managing Inflammatory Conditions: Keeping conditions like ulcerative colitis in check can reduce the risk of inflammatory polyps.
- Diet and Lifestyle: Similar recommendations as for neoplastic polyps.
- Avoid Smoking: Reducing or eliminating tobacco use can decrease the risk.
- Regular Check-ups: Especially for those with inherited conditions or syndromes that raise the risk of polyps.
Preventive strategies focus on modifiable risk factors. It’s essential to note that even with preventive measures, there’s no guarantee of avoiding polyps. Regular check-ups and screenings are crucial, especially for high-risk individuals.
Final Thoughts
Neoplastic and non-neoplastic polyps are growths that arise in various mucosal linings, most commonly within the gastrointestinal tract. Neoplastic polyps have the potential to progress to cancer and are characterized by abnormal cellular changes, necessitating close monitoring and often removal. In contrast, non-neoplastic polyps, which include hyperplastic and inflammatory types, typically lack malignant potential but can cause symptoms in certain situations.
While both types of polyps can share risk factors and diagnostic approaches, their management and implications for long-term health can differ significantly. Regular screening and early detection are paramount in mitigating potential complications and ensuring optimal health outcomes.