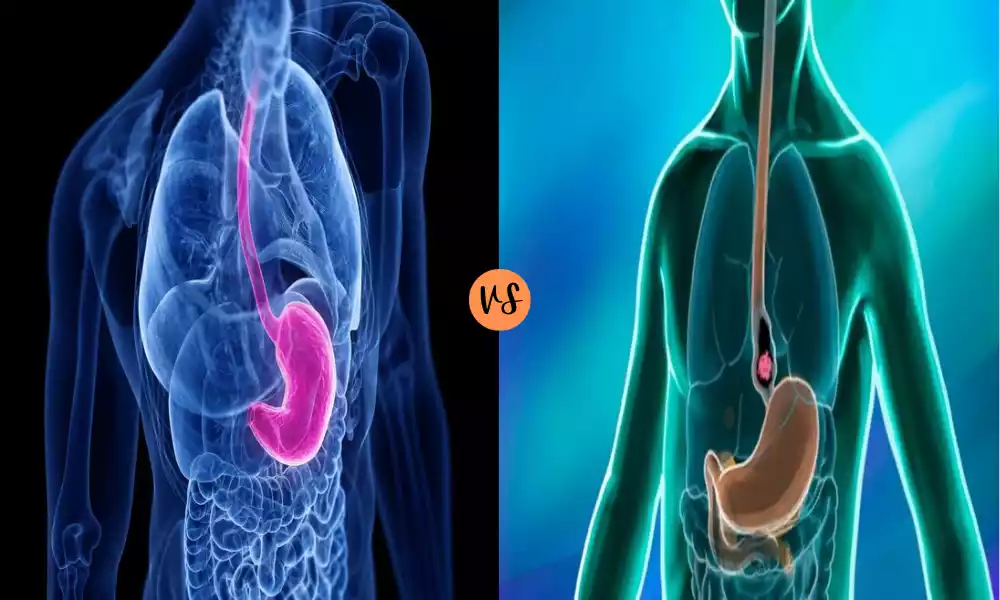
Achalasia and Esophageal Cancer are two distinct conditions affecting the esophagus, the tube that connects the throat to the stomach. Achalasia is a rare disorder characterized by the esophagus’s inability to move food into the stomach effectively, primarily due to the absence or dysfunction of esophageal peristalsis and the failure of the lower esophageal sphincter to relax. In contrast, esophageal cancer is a malignancy arising from the esophagus’s tissues, with its primary types being adenocarcinoma and squamous cell carcinoma.
While both conditions can lead to difficulty swallowing (dysphagia) and other overlapping symptoms, their causes, treatments, and prognoses differ significantly. Early diagnosis and intervention are crucial for both, emphasizing the importance of understanding and recognizing their unique presentations and characteristics.
Definition of Achalasia
Achalasia is a rare and chronic disorder that affects the esophagus, the tube connecting the mouth to the stomach. It’s primarily characterized by two major abnormalities: the lack of effective and coordinated muscle contractions (peristalsis) in the esophagus and the inability of the lower esophageal sphincter (LES) – a muscular ring at the junction of the esophagus and stomach – to relax properly.
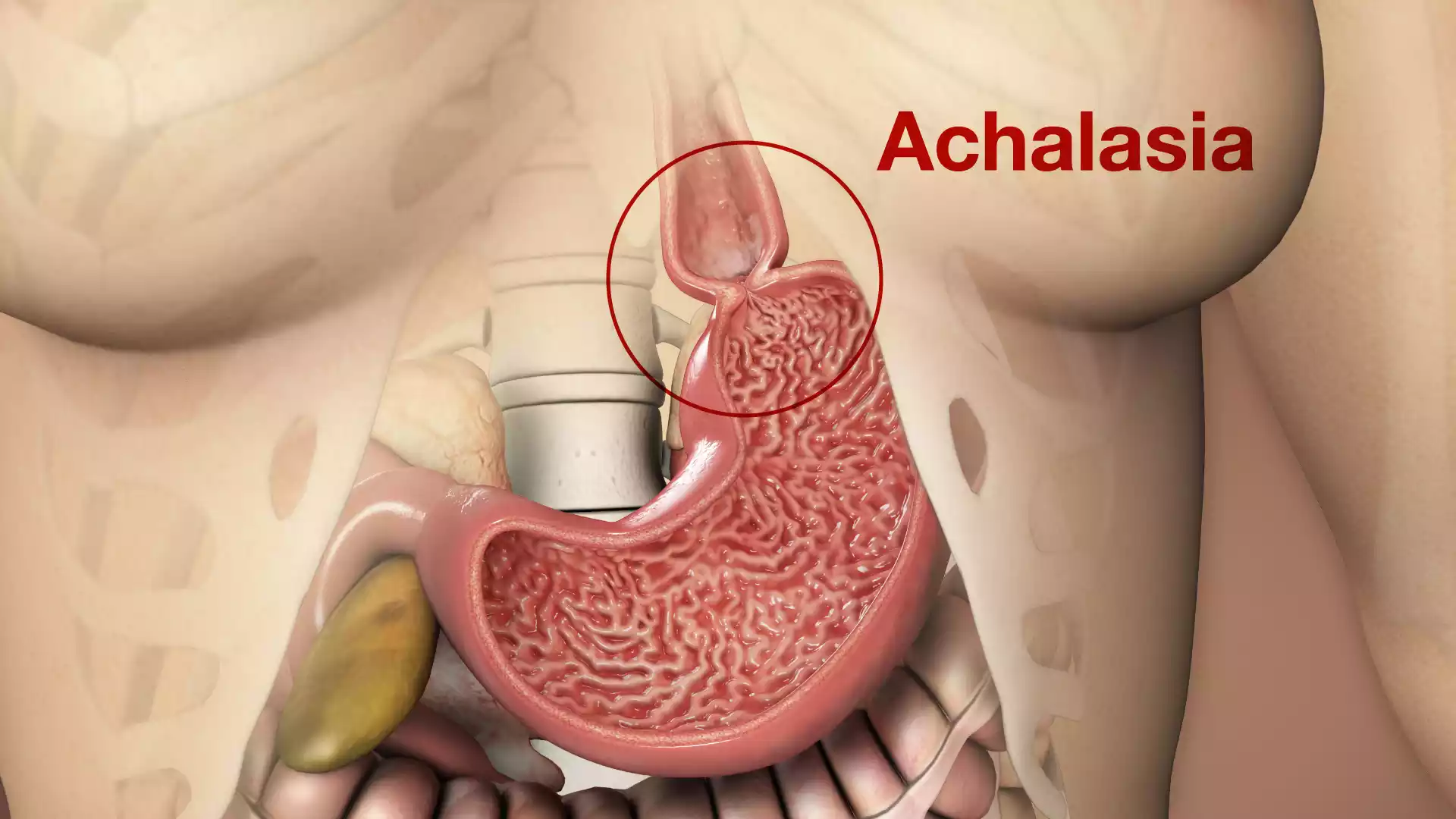
These dysfunctions lead to difficulty in swallowing (dysphagia), regurgitation of food, and often chest pain. While the precise cause of achalasia remains unknown, it’s believed to result from the degeneration of nerve cells in the esophagus.
This degeneration may be due to factors such as a viral infection or an autoimmune response, although the exact triggers are still a subject of research. The condition can significantly impact the quality of life, making timely diagnosis and appropriate treatment essential for affected individuals.
Causes of Achalasia
Achalasia is a disorder of the esophagus characterized by difficulty swallowing due to the absence of esophageal peristalsis and the failure of the lower esophageal sphincter to relax. The exact cause of achalasia remains unclear, but several theories and factors have been proposed:
- Loss of Nerve Cells: The most accepted hypothesis is the degeneration of the nerve cells (ganglion cells) in the esophagus, particularly those that control the lower esophageal sphincter. This results in the muscle’s failure to relax and impaired coordinated contractions.
- Autoimmune Reaction: Some research suggests that the body’s own immune system may attack the esophageal nerve cells, leading to their degeneration. This autoimmune reaction could be triggered by viral infections or other unknown factors.
- Viral Infection: Some studies have found evidence of prior viral infections in patients with achalasia, suggesting that certain viral infections might trigger the disease. However, no specific virus has been conclusively identified as a direct cause.
- Genetic Predisposition: While most cases of achalasia appear to be sporadic, there have been reports of familial clustering, suggesting that genetic factors might play a role in some cases.
- Inflammation: Histological examinations of the esophagus in achalasia patients often reveal inflammation, but whether this is a cause or a result of the disorder is not clear.
- Other Theories: Some less commonly proposed theories include exposure to certain environmental toxins or the possibility of a preceding infection leading to the condition.
Despite these theories, the exact pathogenesis of achalasia remains a topic of ongoing research, and it’s likely that multiple factors contribute to its development in different patients.
Symptoms of Achalasia
Achalasia primarily affects the esophagus, leading to a range of symptoms that stem from the difficulty of food and liquid passing from the esophagus into the stomach. The main symptoms of achalasia include:
- Dysphagia (Difficulty Swallowing): This is the most common symptom. Patients may have difficulty swallowing both solids and liquids. Over time, as the condition progresses, swallowing becomes increasingly difficult.
- Regurgitation: Undigested food and liquids can come back up, especially when lying down. This can also lead to aspiration, where food or liquid enters the lungs, causing coughing or even pneumonia.
- Chest Pain: This can occur during or after eating and can sometimes be severe, often mistaken for heart pain.
- Heartburn: A burning sensation in the chest, which can be mistaken for gastroesophageal reflux disease (GERD), but the cause in achalasia is different.
- Weight Loss: Due to difficulty eating and reduced food intake.
- Cough: Especially at night or when lying down, due to regurgitation.
- Belching.
- Feeling of Food Stuck in the Chest: Often after eating.
- Nocturnal Coughing and Choking: From aspiration of regurgitated food.
While these symptoms can be suggestive of achalasia, they can also be present in other esophageal and gastrointestinal disorders. It’s essential to see a physician for an accurate diagnosis and appropriate management.
Definition of Esophageal Cancer
Esophageal cancer is a malignant tumor that originates in the esophagus, the long, hollow tube that runs from the throat to the stomach, responsible for transporting food and liquids. There are two primary types of esophageal cancer: squamous cell carcinoma, which begins in the flat, thin cells lining the esophagus, and adenocarcinoma, which starts in the glandular cells at the esophagus’s lower end.
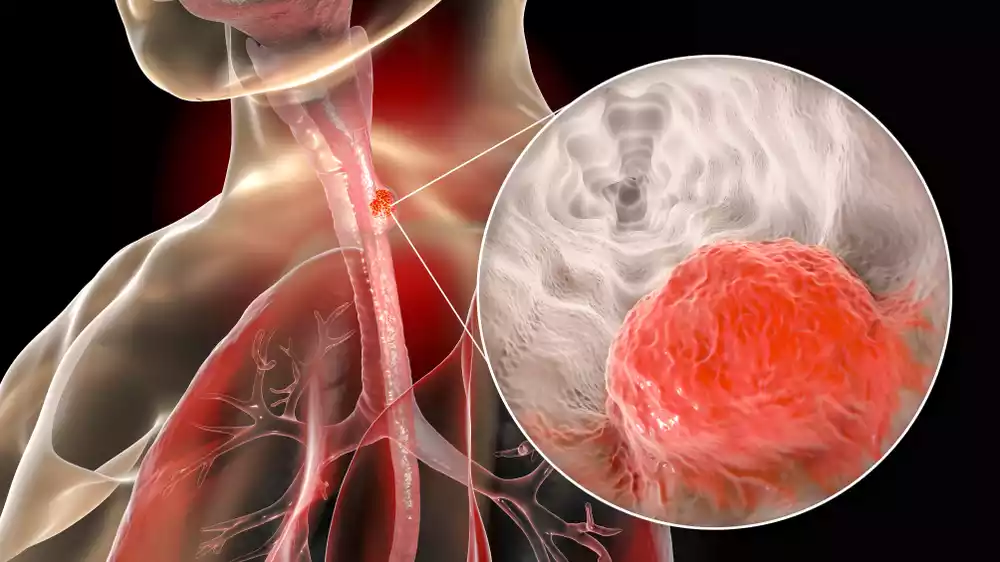
Factors such as tobacco use, heavy alcohol consumption, chronic acid reflux, and conditions like Barrett’s esophagus can increase the risk of developing this cancer. Common symptoms include difficulty swallowing, weight loss, chest pain, hoarseness, and a persistent cough. Early detection and treatment are crucial, as the disease can advance and spread to other parts of the body, complicating treatment and prognosis.
Causes of Esophageal Cancer
Esophageal cancer arises from a series of mutations in esophageal cells, leading to uncontrolled growth and the formation of a tumor. While the exact cause of these mutations is not fully understood, several risk factors have been identified that increase the likelihood of developing esophageal cancer:
- Tobacco and Alcohol Use: Both tobacco smoking (whether cigarettes, cigars, or pipes) and heavy alcohol consumption are significant risk factors, especially for squamous cell carcinoma of the esophagus. The combined effect of smoking and drinking alcohol raises the risk even more.
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux can lead to Barrett’s esophagus, a precancerous condition where the tissue lining the esophagus changes to resemble the lining of the intestine. This condition significantly raises the risk of adenocarcinoma of the esophagus.
- Barrett’s Esophagus: As mentioned, this condition, arising often due to chronic GERD, increases the risk of developing adenocarcinoma.
- Diet: A diet low in fruits and vegetables, or high in processed meats, can increase the risk of esophageal cancer.
- Obesity: Being overweight or obese increases the risk of adenocarcinoma of the esophagus.
- Achalasia: As previously discussed, this esophageal motility disorder can increase the risk of esophageal cancer over time, particularly squamous cell carcinoma.
- Drinking Very Hot Liquids: Regular consumption of scalding hot beverages may increase the risk of squamous cell carcinoma of the esophagus.
- Chemical Exposures: Ingestion of lye (commonly found in drain cleaners) and exposure to certain chemicals used in dry cleaning have been associated with a heightened risk.
- Previous Radiation Treatment: Patients who have had radiation therapy to the chest or upper abdomen can have an increased risk of esophageal cancer.
- Certain Diseases and Conditions: Conditions like Plummer-Vinson syndrome and tylosis are rare but can increase the risk of esophageal cancer.
- Age, Gender, and Race: Older age, being male, and being African American are associated with a higher risk of esophageal cancer.
- Family History: Having a close relative with esophageal cancer can slightly increase the risk.
While these factors can increase the risk of esophageal cancer, not everyone with these risk factors will develop the disease. Conversely, some people with no known risk factors might still develop esophageal cancer. Regular screenings and consultations with healthcare professionals are crucial for those at higher risk.
Symptoms of Esophageal Cancer
Esophageal cancer often does not cause symptoms in its early stages. As the disease progresses, the following symptoms may arise:
- Dysphagia (Difficulty Swallowing): Initially, a person may feel discomfort or a “sticking” sensation when swallowing, which may later progress to significant difficulty. At first, it might be more pronounced with solid foods but can eventually affect liquids as well.
- Unintended Weight Loss: This is often due to decreased food intake because of swallowing difficulties.
- Chest Pain or Discomfort: This might be felt behind the breastbone or between the shoulder blades. It can sometimes be mistaken for heartburn or gastroesophageal reflux.
- Hoarseness: Changes in voice or chronic cough can occur if the tumor affects the laryngeal nerve.
- Chronic Cough: A persistent cough that doesn’t go away can be a symptom.
- Regurgitation of Food: Especially in advanced stages or when there’s a significant obstruction in the esophagus.
- Heartburn or Indigestion: These symptoms can be present in various gastrointestinal diseases, but they can also be associated with esophageal cancer.
- Bleeding in the Esophagus: This can lead to black, tarry stools or vomiting blood.
- Worsening Heartburn or Acid Reflux: Especially if previously managed by over-the-counter medications.
- Respiratory Symptoms: Aspiration of food or liquids due to obstruction can lead to pneumonia or lung problems.
- Feeling of a Lump or Thickness in the Throat: Some people describe a sensation of a growing mass in their throat.
It’s essential to recognize that many of these symptoms can also be caused by conditions other than esophageal cancer, such as GERD, achalasia, or infections. However, if these symptoms are persistent or severe, they should be evaluated by a physician. Early detection and treatment can have a significant impact on the prognosis of esophageal cancer.
Comparison Table of Achalasia and Esophageal Cancer
Here’s a comparison table highlighting the differences between Achalasia and Esophageal Cancer:
| Feature | Achalasia | Esophageal Cancer |
|---|---|---|
| Definition | A disorder affecting esophageal motility. | A malignant tumor originating in the esophagus. |
| Primary Issue | Ineffective esophageal peristalsis and LES failure to relax | Uncontrolled cell growth in the esophagus. |
| Main Types | N/A | 1. Squamous cell carcinoma 2. Adenocarcinoma |
| Causes | Unknown, possibly nerve damage or autoimmune reactions. | Tobacco use, alcohol, GERD, Barrett’s esophagus, etc. |
| Symptoms | Difficulty swallowing, regurgitation, chest pain. | Difficulty swallowing, weight loss, chest pain, hoarseness. |
| Risk Factors | Not well-defined. | Smoking, alcohol, chronic acid reflux, dietary patterns. |
| Diagnosis | Esophageal manometry, barium swallow study, endoscopy. | Endoscopy with biopsy, barium swallow, CT, PET scans. |
| Treatment | Medications, balloon dilation, Heller myotomy, Botox. | Surgery, radiation, chemotherapy, targeted therapies. |
| Prognosis | Non-malignant, quality of life affected, but not life-threatening. | Depends on stage; can be life-threatening if not treated early. |
This table provides a general comparison and may not capture all aspects or nuances of the conditions. Always consult with a healthcare professional for a comprehensive understanding and diagnosis.
Diagnosis of Achalasia and Esophageal Cancer
Achalasia and esophageal cancer both affect the esophagus, but their diagnostic processes differ due to their distinct nature. Here’s a summary of the diagnostic procedures for each condition:
Achalasia:
- Barium Swallow (Esophagram): The patient swallows a liquid containing barium, which outlines the esophagus on X-rays. In achalasia, a “bird’s beak” appearance can be observed due to the narrowing at the lower esophageal sphincter (LES) and dilation of the esophagus above it.
- Esophageal Manometry: The gold standard for achalasia diagnosis. It measures the muscle contractions inside the esophagus and the relaxation of the LES. Achalasia will show the absence of normal esophageal peristalsis and failure of the LES to relax.
- Endoscopy (Esophagogastroduodenoscopy, EGD): A flexible tube with a camera is inserted down the throat to inspect the esophagus and stomach. It can rule out other causes of dysphagia and confirm the presence of food retention. However, it cannot definitively diagnose achalasia by itself.
- pH Monitoring: Helps differentiate achalasia from GERD (gastroesophageal reflux disease) as the cause of symptoms.
- Chest CT scan or MRI: Occasionally used to rule out other conditions or if there’s a suspicion of malignancy.
Esophageal Cancer:
- Endoscopy (Esophagogastroduodenoscopy, EGD): Similar to its use in achalasia diagnosis, EGD allows for visual inspection of the esophagus. Any suspicious areas can be biopsied during this procedure.
- Biopsy: Tissue samples taken during an endoscopy are examined under a microscope to determine if cancer cells are present and to identify the type of cancer (either squamous cell carcinoma or adenocarcinoma).
- Barium Swallow (Esophagram): Helps visualize tumors or any narrowing in the esophagus.
- Endoscopic Ultrasound (EUS): Assesses how deeply the cancer has invaded the esophageal layers and whether nearby lymph nodes are involved.
- Computed Tomography (CT) Scan: Checks for cancer spread to nearby structures or distant organs, like the lungs or liver.
- Positron Emission Tomography (PET) Scan: Can detect areas of increased metabolic activity, indicating possible cancer spread.
- Magnetic Resonance Imaging (MRI): Occasionally used for detailed images of the esophagus and surrounding structures.
- Bronchoscopy: If there’s a suspicion that the tumor has invaded the trachea or bronchi, or if there’s concern about possible cancer spread to the lungs.
The differential diagnosis is essential as these conditions have different treatment protocols and prognoses. While both can present with dysphagia, their management and implications are vastly different. Early and accurate diagnosis is crucial for appropriate treatment and improved outcomes.
Treatment Approach for Achalasia and Esophageal Cancer
Both achalasia and esophageal cancer involve the esophagus, but they are distinct diseases with different treatment approaches. Here’s an overview of treatment modalities for each condition:
Achalasia:
The primary goal of treating achalasia is to reduce symptoms, particularly dysphagia, by relieving the obstruction at the lower esophageal sphincter (LES).
- Pneumatic Dilation: This involves placing a balloon at the LES and inflating it to stretch and weaken the muscle. This procedure is typically done under sedation.
- Botulinum Toxin (Botox) Injection: Botox can be injected into the LES during an endoscopy to weaken the muscle. This is often a temporary solution and might be used for individuals who aren’t good candidates for other therapies.
- Heller Myotomy: A surgical procedure where the muscles of the LES are cut to allow it to remain open. This can be performed laparoscopically in most cases.
- Peroral Endoscopic Myotomy (POEM): A newer, less invasive procedure where an endoscope is used to create an incision in the inner lining of the esophagus and then cut the LES muscle.
- Medications: Some drugs, like nitrates or calcium channel blockers, can relax the LES, but they offer temporary relief and aren’t as effective as other treatments.
- Esophagectomy: In very severe cases, removing a part or the entire esophagus may be necessary, though this is a rare approach.
Esophageal Cancer:
Treatment of esophageal cancer depends on the type of cancer (adenocarcinoma or squamous cell carcinoma), its stage, location, and the patient’s overall health.
- Surgery:
- Esophagectomy: Removal of all or part of the esophagus.
- Esophagogastrectomy: Removal of the upper part of the stomach and part of the esophagus.
- Radiation Therapy: High doses of radiation are used to kill or shrink cancer cells.
- Chemotherapy: Drugs are used to kill cancer cells or stop them from growing. It can be given before surgery (neoadjuvant) to shrink the tumor or after surgery (adjuvant) to kill any remaining cancer cells.
- Targeted Therapy: Uses drugs to target specific molecules involved in cancer growth.
- Immunotherapy: Uses the body’s immune system to recognize and attack cancer cells.
- Endoscopic Therapies: For early-stage cancers or precancerous lesions, techniques like endoscopic mucosal resection (EMR) or radiofrequency ablation (RFA) might be used.
- Palliative Care: In advanced stages where curative treatment isn’t possible, the focus shifts to relieving symptoms and improving quality of life.
In both conditions, a multidisciplinary approach involving gastroenterologists, surgeons, oncologists (for cancer), radiologists, and other healthcare professionals is essential for optimal management. Regular follow-up and monitoring are also crucial, especially after treatments, to check for recurrence or complications.
Living with Achalasia and Esophageal Cancer
Living with achalasia or esophageal cancer presents unique challenges and requires adjustments to one’s daily life. Here’s an overview of what it’s like living with each condition and some general coping strategies:
Living with Achalasia:
- Dietary Changes: Patients often need to modify their eating habits:
- Eat slowly.
- Take small bites and chew thoroughly.
- Drink fluids during meals to help food pass.
- Elevate the head of the bed to prevent nighttime regurgitation.
- Regular Monitoring: Regular follow-ups with a gastroenterologist are necessary to monitor symptom progression and treatment efficacy.
- Physical Impact: While treatments can alleviate symptoms, some patients may still experience intermittent difficulty swallowing, chest pain, or regurgitation.
- Emotional Impact: The chronic nature of achalasia and the dietary restrictions can lead to feelings of isolation, especially during social events centered around food.
Living with Esophageal Cancer:
- Treatment Side Effects: Treatments like chemotherapy, radiation, and surgery can have side effects such as fatigue, pain, difficulty swallowing, or nutritional challenges.
- Nutritional Challenges: Due to swallowing difficulties or surgical alterations, patients might require:
- Soft or liquid diets.
- Nutritional supplements or feeding tubes in severe cases.
- Regular Medical Visits: Frequent appointments for treatment, monitoring, and follow-up are a part of life with esophageal cancer.
- Emotional and Psychological Impact: Being diagnosed with cancer can be overwhelming. Feelings of anxiety, depression, and fear are common.
- Support: Joining support groups or seeking psychological therapy can be beneficial. Interacting with others who’ve had similar experiences provides comfort and understanding.
General Coping Strategies:
- Stay Informed: Understanding the condition can help in making informed decisions about treatments and lifestyle adjustments.
- Seek Support: Whether it’s from family, friends, support groups, or professional therapists, having a support system is essential.
- Maintain a Balanced Diet: For both conditions, nutritional intake is crucial. Consulting with a nutritionist can help in crafting a diet plan suitable for specific needs.
- Stay Active: Engage in mild physical activities, as recommended by the healthcare provider, to maintain overall health and well-being.
- Communicate with Healthcare Providers: Regularly discuss symptoms, concerns, and any changes in health status.
Living with either achalasia or esophageal cancer necessitates significant lifestyle changes and adjustments. A proactive approach to management, coupled with a robust support system, can significantly enhance the quality of life and overall well-being.
Conclusion
Achalasia and Esophageal Cancer are distinct disorders affecting the esophagus, each with its unique etiology, presentation, and management. Achalasia is a motility disorder characterized by the failure of the lower esophageal sphincter to relax, leading to difficulty swallowing and other symptoms. In contrast, esophageal cancer is a malignant condition, with squamous cell carcinoma and adenocarcinoma being the most common types.
Both conditions can present with dysphagia, making a differential diagnosis vital. While they share some diagnostic tools, their treatments diverge significantly. It’s crucial to understand the differences between these conditions for timely and appropriate medical intervention, ensuring optimal patient outcomes.