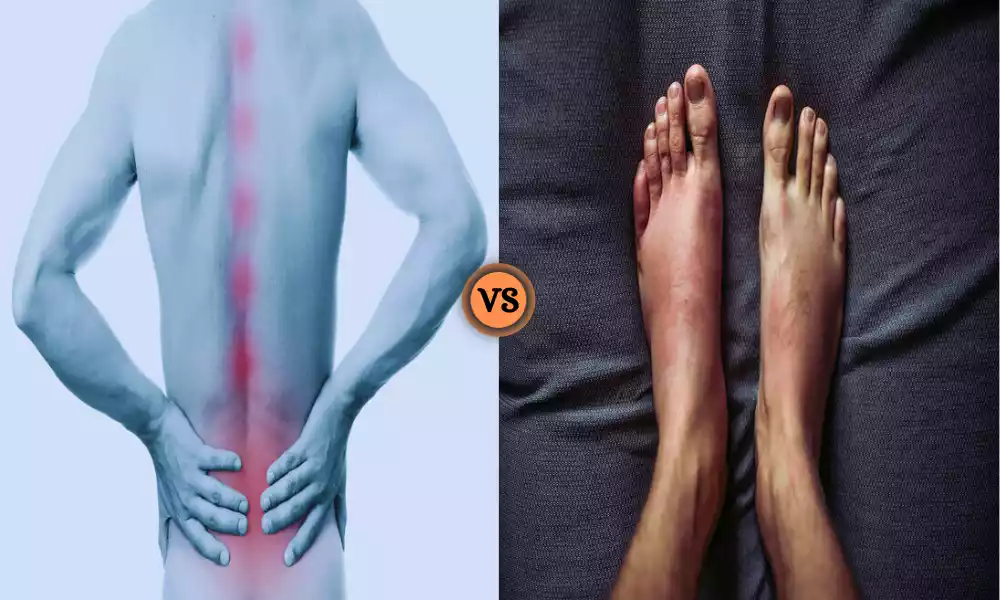
Ankylosing Spondylitis and Psoriatic Arthritis are two distinct autoimmune conditions that affect the musculoskeletal system. AS primarily targets the spine, causing chronic pain and reduced mobility, while PsA is associated with joint inflammation and often co-occurs with psoriasis, a skin condition. Despite their differences, both conditions share the potential for debilitating symptoms and require early diagnosis and tailored treatment approaches to improve patients’ quality of life.
Definition of Ankylosing Spondylitis
Ankylosing Spondylitis (AS) is a chronic and progressive autoimmune inflammatory disorder primarily affecting the spine and sacroiliac joints. It belongs to a group of conditions known as spondyloarthropathies.

AS causes inflammation of the vertebrae (the bones of the spine) and can lead to pain, stiffness, and in severe cases, fusion of the spinal joints, resulting in reduced flexibility and mobility of the spine. It often begins in early adulthood and can also involve other joints and organs, leading to various symptoms and complications.
Symptoms of Ankylosing Spondylitis
Ankylosing Spondylitis (AS) can present with a range of symptoms that typically develop gradually and vary among individuals. Common symptoms of AS include:
-
- Chronic Lower Back Pain: Persistent and progressive pain and stiffness in the lower back are often the earliest and most prominent symptoms. This pain is usually worse in the morning or after periods of inactivity and may improve with exercise and movement.
- Stiffness: Stiffness in the back and neck, particularly in the morning or after prolonged periods of rest or inactivity, is a hallmark symptom of AS.
- Reduced Spinal Mobility: AS can lead to a loss of flexibility in the spine, which can result in difficulty bending or turning the spine.
- Pain and Swelling in Other Joints: While primarily a spinal condition, AS can also affect other joints, such as the hips, knees, shoulders, and ankles, causing pain, swelling, and reduced joint mobility.
- Enthesitis: Inflammation at the sites where tendons and ligaments attach to bones (entheses) can lead to pain and tenderness, often at the heels, chest wall, or other locations.
- Fatigue: Many individuals with AS experience fatigue, which can be both a symptom of the condition itself and a result of disrupted sleep due to pain and discomfort.
- Weight Loss and Loss of Appetite: Some people with AS may experience unintentional weight loss and a decreased appetite, particularly during disease flares.
- Eye Inflammation: A condition called anterior uveitis or iritis, which involves inflammation of the eye, can occur in people with AS and can cause eye pain, redness, and sensitivity to light.
- Breathing Difficulties: In severe cases, AS can lead to reduced chest expansion due to the fusion of the rib joints to the spine, potentially leading to breathing difficulties.
- Other Systemic Symptoms: AS is associated with an increased risk of other conditions, such as inflammatory bowel disease, cardiovascular issues, and osteoporosis.
The severity and combination of symptoms can vary widely from person to person. Early diagnosis and appropriate management, often involving medications and physical therapy, can help individuals with AS manage their symptoms and maintain a good quality of life.
Definition of Psoriatic Arthritis
Psoriatic Arthritis (PsA) is a chronic inflammatory joint condition that occurs in some individuals who have the skin disorder psoriasis. It is categorized as an autoimmune disease, as the immune system mistakenly targets and attacks healthy joints and tissues. Psoriatic Arthritis typically affects the joints, causing pain, swelling, and stiffness.

This condition can vary in its presentation and severity, affecting not only the joints but also potentially causing inflammation of the skin, nails, eyes, and other organs. The symptoms of Psoriatic Arthritis can range from mild to severe, and early diagnosis and treatment are crucial in managing the disease and preventing joint damage.
Symptoms of Psoriatic Arthritis
Psoriatic Arthritis (PsA) can manifest with a wide range of symptoms that affect both the joints and other parts of the body. These symptoms may vary among individuals, but common signs and symptoms of Psoriatic Arthritis include:
-
- Joint Pain: Persistent pain and discomfort in one or more joints, often with a “stinging” or “burning” sensation.
- Joint Swelling: Swelling and inflammation in the affected joints, which can lead to joint stiffness and reduced mobility.
- Morning Stiffness: Stiffness in the affected joints, usually worse in the morning or after periods of rest.
- Skin Changes: In many cases, PsA is associated with psoriasis, a chronic skin condition characterized by red, scaly patches. Psoriasis symptoms can precede, coincide with, or follow the onset of PsA.
- Nail Changes: Psoriatic Arthritis can cause nail problems, such as pitting, ridges, or discoloration, known as psoriatic nail dystrophy.
- Tendon or Ligament Pain: Pain and inflammation in the tendons or ligaments surrounding the joints, a condition referred to as enthesitis.
- Dactylitis: Swelling of an entire finger or toe, giving it a sausage-like appearance.
- Fatigue: Chronic fatigue and a feeling of general tiredness.
- Eye Inflammation: Inflammation of the eye, called uveitis or iritis, which can cause eye pain, redness, and sensitivity to light.
- Lower Back Pain: Some individuals with PsA may experience lower back pain, resembling symptoms of ankylosing spondylitis.
- Gastrointestinal Symptoms: Inflammatory bowel disease, such as Crohn’s disease or ulcerative colitis, can occur alongside PsA.
- Tenderness: Tender areas around the joints, especially where ligaments and tendons attach to bones.
- Reduced Range of Motion: Decreased flexibility and limited range of motion in the affected joints.
- Generalized Symptoms: In severe cases, individuals with PsA may experience fever and general malaise.
Psoriatic Arthritis (PsA) is a highly variable condition, and not all individuals will experience the same combination or severity of symptoms. Early diagnosis and appropriate treatment are essential to manage symptoms, prevent joint damage, and improve the quality of life for individuals with Psoriatic Arthritis.
Comparison Table of Ankylosing Spondylitis and Psoriatic Arthritis
Here’s a comparison table highlighting the key differences and some similarities between Ankylosing Spondylitis (AS) and Psoriatic Arthritis (PsA):
| Aspect | Ankylosing Spondylitis (AS) | Psoriatic Arthritis (PsA) |
|---|---|---|
| Definition | Chronic autoimmune inflammatory disorder primarily affecting the spine and sacroiliac joints. | Chronic inflammatory joint condition occurring in individuals with psoriasis. |
| Predominant Symptoms | – Chronic lower back pain and stiffness
– Reduced spinal mobility – Enthesitis (tendon and ligament inflammation) |
– Joint pain and swelling
– Skin psoriasis – Nail changes (psoriatic nail dystrophy) |
| Age of Onset | Typically begins in early adulthood. | Can develop at any age, but most commonly diagnosed in people aged 30 to 50. |
| Joint Involvement | Mainly affects the spine and sacroiliac joints, but can also involve peripheral joints. | Affects various joints, including peripheral joints like fingers, toes, knees, and hips. |
| Radiographic Findings | Bamboo spine (fusion of vertebrae), sacroiliitis (inflammation of sacroiliac joints). | Joint erosions, periarticular bone proliferation (“pencil-in-cup” deformity). |
| Skin and Nail Involvement | Typically not associated with skin or nail psoriasis. | Often associated with skin psoriasis and psoriatic nail changes. |
| Extra-Articular Manifestations | Enthesitis, uveitis, and sometimes heart and lung involvement. | Enthesitis, skin psoriasis, nail changes, and eye inflammation (uveitis). |
| Diagnostic Criteria | ASAS criteria, often involving imaging like X-rays or MRI. | CASPAR criteria, which consider joint, skin, and nail involvement. |
| Association with Psoriasis | Usually not associated with psoriasis. | Commonly occurs in individuals with psoriasis (skin condition). |
| Genetic Predisposition | Strong genetic component, especially HLA-B27 gene. | Genetic factors play a role, but HLA-B27 is less commonly associated. |
| Treatment | Medications (NSAIDs, DMARDs), physical therapy, exercise, and sometimes biologics or surgery. | Medications (NSAIDs, DMARDs), biologics, lifestyle modifications, and skin treatments for psoriasis. |
| Prognosis | Varies, but with early diagnosis and treatment, many individuals can lead active lives. | Variable, depending on severity and response to treatment. |
| Impact on Quality of Life | Reduced spinal flexibility and mobility can impact daily life and functionality. | Joint pain and skin issues can affect daily life; fatigue may also be a factor. |
This table provides an overview of the key differences and some similarities between Ankylosing Spondylitis and Psoriatic Arthritis. Keep in mind that the presentation of these conditions can vary from person to person, and individual experiences may differ. Early diagnosis and appropriate treatment are crucial for managing both conditions effectively.
How to Diagnosis of Ankylosing Spondylitis and Psoriatic Arthritis
The diagnosis of Ankylosing Spondylitis (AS) and Psoriatic Arthritis (PsA) typically involves a combination of clinical evaluation, medical history, physical examination, and various diagnostic tests. Here’s an overview of the diagnostic process for both conditions:
Diagnosis of Ankylosing Spondylitis (AS):
- Clinical Assessment: The diagnosis begins with a thorough evaluation by a rheumatologist or other healthcare provider. They will assess your symptoms, medical history, and family history of AS or related conditions.
- Physical Examination: The healthcare provider will perform a physical examination to look for signs of inflammation, joint stiffness, and any limitations in spinal mobility. They may also check for enthesitis (inflammation at tendon and ligament attachments) and other associated features.
- Imaging Studies:
- X-rays: X-rays of the spine and sacroiliac joints may reveal characteristic findings, such as bamboo spine (fusion of vertebrae) or sacroiliitis (inflammation of the sacroiliac joints).
- MRI (Magnetic Resonance Imaging): An MRI can provide more detailed images of the spine and sacroiliac joints, especially in the early stages of AS.
- Blood Tests: Although there is no specific blood test to diagnose AS, some markers like HLA-B27 antigen are associated with the condition. However, HLA-B27 is not exclusive to AS and may be present in healthy individuals as well.
- Assessment of Disease Activity: Various tools and questionnaires, such as the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), are used to assess disease activity and monitor response to treatment.
Diagnosis of Psoriatic Arthritis (PsA):
- Clinical Assessment: Similar to AS, PsA diagnosis starts with a comprehensive clinical evaluation by a rheumatologist or dermatologist. A history of psoriasis or a family history of psoriasis and PsA is considered.
- Physical Examination: The healthcare provider will conduct a physical examination to identify signs of joint inflammation, skin psoriasis, nail changes, and other relevant symptoms. Particular attention is given to affected joints, including those in the hands, feet, and spine.
- Imaging Studies:
- X-rays: X-rays of affected joints may show joint erosions or periarticular bone changes, which are indicative of PsA.
- Ultrasound or MRI: These imaging techniques can provide more detailed images of joint inflammation and damage.
- Blood Tests: While there is no specific blood test for PsA, tests may be done to rule out other conditions and assess inflammation markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
- Skin and Nail Examination: A dermatologist may examine the skin and nails for psoriasis or psoriatic nail changes, which are common features of PsA.
- Assessment of Disease Activity: Tools like the Psoriatic Arthritis Disease Activity Score (PASDAS) or the Disease Activity in Psoriatic Arthritis (DAPSA) are used to assess disease activity and monitor treatment effectiveness.
- Exclusion of Other Conditions: Sometimes, other conditions with similar symptoms, such as rheumatoid arthritis, must be ruled out through diagnostic tests.
Both AS and PsA can be challenging to diagnose because their symptoms can overlap with other conditions. Therefore, it’s crucial to consult a healthcare professional experienced in rheumatology or dermatology for an accurate diagnosis and appropriate management. Early diagnosis and treatment are essential to minimize joint damage and improve the quality of life for individuals with these conditions.
Treatment approaches for Ankylosing Spondylitis and Psoriatic Arthritis
The treatment approaches for Ankylosing Spondylitis (AS) and Psoriatic Arthritis (PsA) aim to manage symptoms, reduce inflammation, improve joint function, and enhance the overall quality of life for individuals with these conditions. The treatment plans are typically tailored to the specific needs and severity of each patient.
Here’s an overview of the treatment approaches for AS and PsA:
Treatment for Ankylosing Spondylitis (AS):
- Medications:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs like ibuprofen and naproxen can help relieve pain and reduce inflammation. They are often the first line of treatment.
- Disease-Modifying Antirheumatic Drugs (DMARDs): In some cases, DMARDs like sulfasalazine may be prescribed to slow down the progression of AS.
- Biologic Agents: Biologics, such as tumor necrosis factor (TNF) inhibitors (e.g., adalimumab, etanercept), are used for moderate to severe AS when NSAIDs and DMARDs are ineffective.
- Physical Therapy: Physical therapy and exercises, particularly ones aimed at maintaining spinal flexibility and posture, are crucial for managing AS. A physical therapist can provide a tailored exercise program.
- Lifestyle Modifications: Lifestyle changes such as quitting smoking and maintaining a healthy weight can help improve AS symptoms.
- Pain Management: For severe pain, pain management techniques such as epidural steroid injections may be considered.
- Surgery: In rare cases, surgical procedures may be needed to correct severe deformities or joint damage. Examples include joint replacement surgery or spinal fusion.
- Disease Education: Education about the condition, self-care, and strategies for managing symptoms is an important aspect of AS treatment.
Treatment for Psoriatic Arthritis (PsA):
- Medications:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs are commonly used to reduce pain and inflammation.
- Disease-Modifying Antirheumatic Drugs (DMARDs): DMARDs like methotrexate are prescribed to slow the progression of joint damage in PsA.
- Biologic Agents: Biologics, including TNF inhibitors (e.g., etanercept, adalimumab) and other targeted therapies, are often used for moderate to severe PsA to control inflammation and slow joint damage.
- Physical Therapy: Physical therapy and specific exercises can help improve joint function, maintain mobility, and strengthen muscles around affected joints.
- Skin and Nail Treatments: Dermatologists may recommend treatments for skin psoriasis and psoriatic nail changes, which can include topical therapies, phototherapy, or systemic medications.
- Lifestyle Modifications: Lifestyle changes such as regular exercise, maintaining a healthy weight, and managing stress can help manage PsA symptoms.
- Pain Management: Pain management strategies, including joint injections with corticosteroids, can provide relief for painful joints.
- Surgery: In advanced cases of PsA with severe joint damage, surgical interventions like joint replacement surgery may be necessary.
- Patient Education: Patients benefit from understanding their condition, including triggers and lifestyle choices that may impact symptoms.
- Monitoring: Regular follow-up appointments with healthcare providers are important for tracking disease activity, adjusting treatments, and ensuring optimal management.
Both conditions may require ongoing treatment and management, and individuals with AS or PsA should work closely with a healthcare team, including rheumatologists, dermatologists (for PsA with skin involvement), and physical therapists, to develop a comprehensive treatment plan tailored to their specific needs. Early diagnosis and proactive management can help individuals with AS and PsA lead healthier, more active lives.
What are the Similarities Ankylosing Spondylitis and Psoriatic Arthritis?
Ankylosing Spondylitis (AS) and Psoriatic Arthritis (PsA) are both types of inflammatory arthritis that share some similarities, even though they have distinct features. Here are the key similarities between the two conditions:
- Inflammatory Nature: Both AS and PsA are chronic inflammatory conditions. In both diseases, the body’s immune system is overactive and attacks its tissues, leading to inflammation in the joints and other areas.
- Affect Multiple Joints: Both conditions can affect multiple joints in the body, not just the spine. While AS primarily affects the spine and sacroiliac joints, it can also involve peripheral joints. PsA, on the other hand, can affect various joints, including the fingers, toes, knees, and hips.
- Symptoms: Both AS and PsA can cause symptoms such as joint pain, swelling, and stiffness. Morning stiffness is a common symptom in both conditions.
- Extra-Articular Manifestations: Both diseases can have extra-articular (outside the joints) manifestations. For example, both AS and PsA can lead to enthesitis (inflammation at tendon and ligament attachments), uveitis (eye inflammation), and heart and lung involvement in severe cases.
- Chronic and Progressive: Both AS and PsA are chronic conditions that tend to progress over time. Without appropriate management, they can lead to joint damage and reduced function.
- Quality of Life Impact: Both conditions can significantly impact an individual’s quality of life due to chronic pain, fatigue, and limitations in mobility.
- Response to Medications: While the specific medications used may differ, both AS and PsA often respond to non-steroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation. Additionally, disease-modifying antirheumatic drugs (DMARDs) and biologics may be used in the treatment of both conditions.
- Importance of Early Diagnosis: Early diagnosis and intervention are crucial in managing both AS and PsA to prevent joint damage and improve outcomes.
While these conditions share similarities, they also have distinct features, such as the association of PsA with skin psoriasis and nail changes, which are not seen in AS. Additionally, the management and treatment approaches may differ between the two conditions based on their unique characteristics. Therefore, a proper diagnosis by a healthcare professional experienced in rheumatology or dermatology is essential for appropriate management.
Conclusion
Ankylosing Spondylitis (AS) and Psoriatic Arthritis (PsA) are chronic inflammatory conditions that affect the joints and can significantly impact the lives of those affected. While both share similarities in terms of inflammation, joint involvement, and the importance of early diagnosis and treatment, they also have distinct features, such as the association of PsA with skin psoriasis and nail changes.
Proper diagnosis and a tailored treatment plan, often involving medications, physical therapy, and lifestyle adjustments, are crucial in managing these conditions and improving the quality of life for individuals living with AS and PsA. Early intervention and ongoing medical care play key roles in minimizing joint damage and maximizing mobility and well-being.