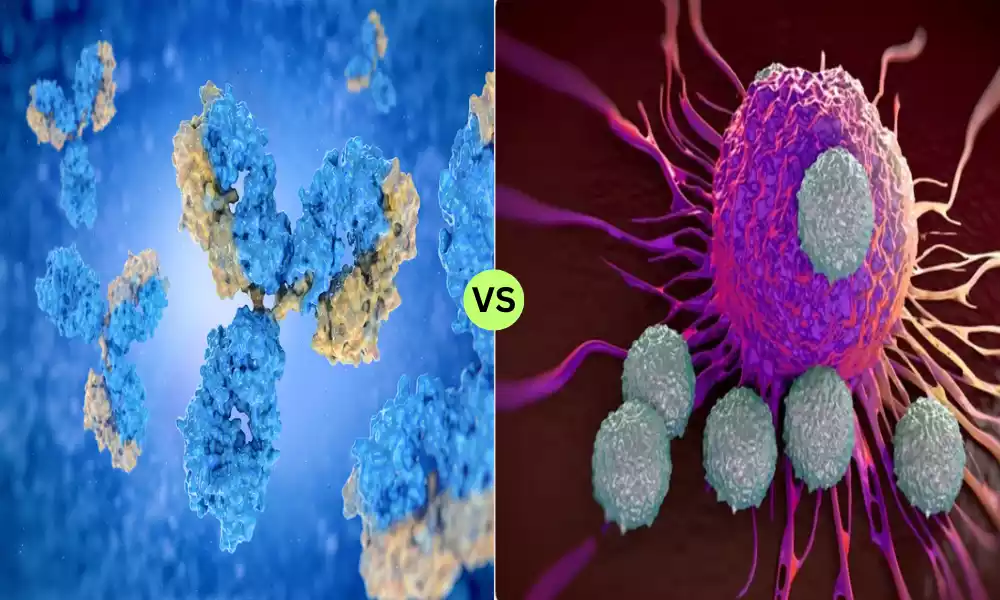
Introduction of Antibodies and T Cells
The immune system stands as a remarkable sentinel, defending the body against foreign invaders and harmful substances. Central to this defense mechanism are antibodies and T cells, two key components that operate with distinct yet interconnected roles. Antibodies are specialized Y-shaped proteins produced by B cells, designed to recognize and neutralize specific pathogens like bacteria and viruses.
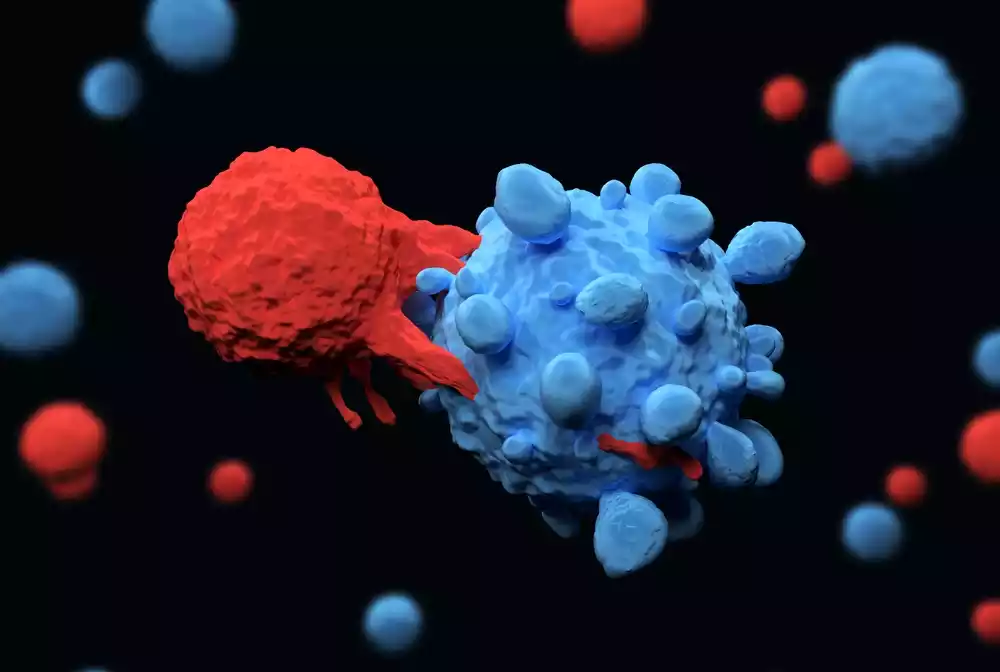
T cells, on the other hand, are a type of white blood cell matured in the thymus, responsible for directly attacking infected cells and orchestrating the broader immune response. Together, they form an intricate web of defense, ensuring our body’s resilience and ability to recover from various threats.
What are Antibodies?
Antibodies, also known as immunoglobulins, are Y-shaped proteins produced by the immune system to identify and neutralize foreign objects such as bacteria, viruses, and other pathogens. They are generated by specialized white blood cells called B lymphocytes, or B cells. Antibodies have a specific structure composed of two heavy chains and two light chains, forming a “Y” shape.
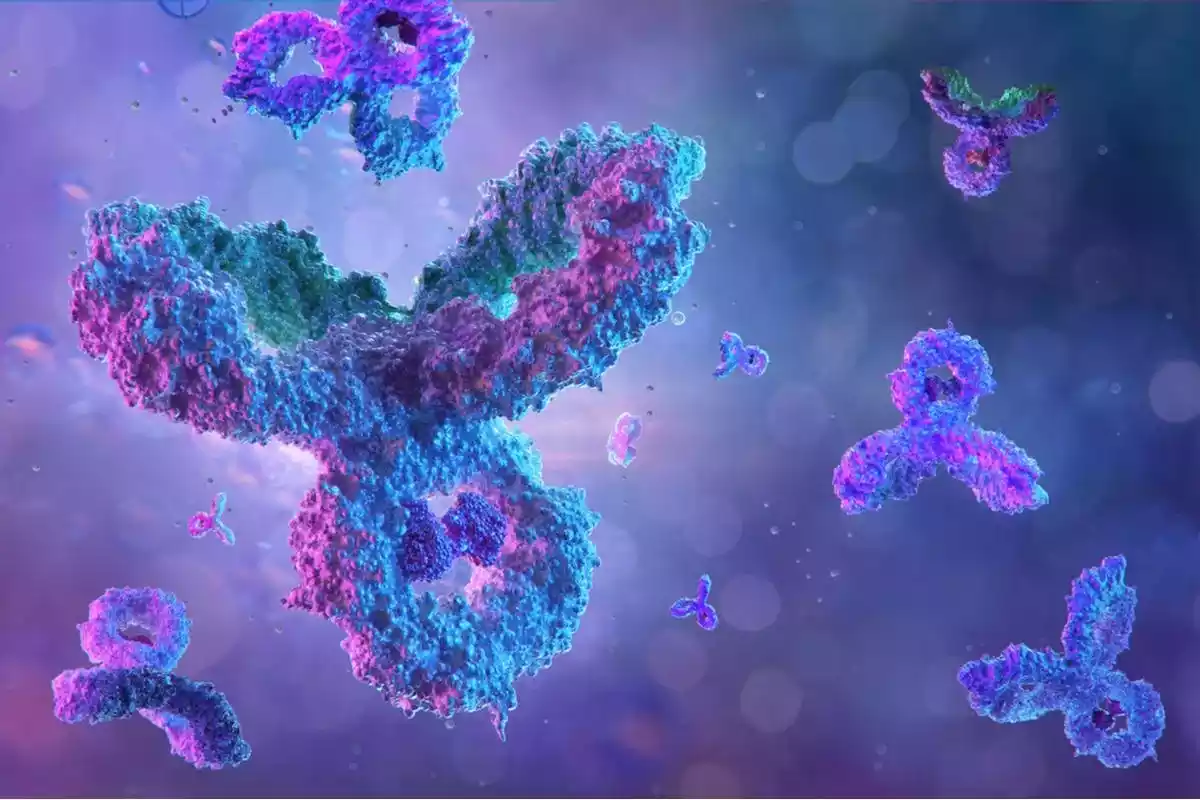
The arms of the ‘Y’ contain regions known as antigen-binding sites, which are capable of recognizing and binding to specific antigens—a term used to describe any substance that can be targeted by an immune response.
Types of Antibodies
There are five main types of antibodies, each with a different function and location within the body:
- IgG: The most abundant type, found in blood and tissue fluids; provides long-term immunity.
- IgA: Found mainly in the mucous membranes lining the gut and respiratory tract, as well as in saliva and tears.
- IgM: The first antibodies to appear in response to an initial exposure to an antigen.
- IgD: Mostly found on the surface of B cells; function not entirely understood.
- IgE: Involved in allergic reactions; found in the lungs, skin, and mucous membranes.
Modes of Action
Antibodies work in several ways:
- Neutralization: They can bind to the pathogens and neutralize their effects.
- Opsonization: They mark pathogens for destruction by other immune cells.
- Activation of the Complement System: They can initiate a cascade of reactions that result in the rupture and death of the pathogen.
Memory and Duration
B cells that produce effective antibodies against a pathogen become memory B cells. These cells can live for years and produce antibodies quickly if the same pathogen is encountered again, providing long-term immunity.
Antibodies are crucial components of the adaptive immune system, providing specificity, memory, and a multi-pronged approach to identifying and neutralizing pathogens.
What are T cells?
T cells, or T lymphocytes, are a type of white blood cell that plays a crucial role in the immune system, particularly in the adaptive immune response. These cells originate from hematopoietic stem cells in the bone marrow but migrate to the thymus—an organ situated between the lungs and the breastbone—for maturation. Unlike antibodies, which are free-floating proteins, T cells are actual cells capable of various functions based on their subtype.
Types of T cells
There are several types of T cells, each with specific roles:
- Helper T Cells (CD4+ T Cells): These cells assist other white blood cells in immunologic processes, including maturation of B cells into plasma cells and memory B cells, and activation of cytotoxic T cells and macrophages.
- Cytotoxic T Cells (CD8+ T Cells): These cells are responsible for directly destroying cells that are infected by viruses or have become cancerous.
- Regulatory T Cells (Tregs): These cells help regulate the immune response, preventing autoimmune diseases by suppressing other immune cells that mistakenly target the body’s own tissues.
- Memory T Cells: Similar to memory B cells, these T cells remain in the body long-term. They enable a faster and more efficient response to pathogens that the body has previously encountered.
Modes of Action
T cells have various modes of action based on their subtype:
- Direct Killing: Cytotoxic T cells identify and kill infected cells directly.
- Coordination: Helper T cells coordinate the immune response by secreting cytokines and other signaling molecules.
- Suppression: Regulatory T cells suppress immune responses, particularly against the body’s own tissues.
- Memory: Memory T cells provide long-term immunity by remaining in the body to respond more quickly upon future exposure to the same pathogen.
T cells offer a multi-faceted approach to adaptive immunity. They are capable of both direct action against infected or malignant cells and orchestration of broader immune responses, making them indispensable in the body’s fight against a wide range of diseases.
Comparison Table of Antibodies and T Cells
Certainly, a comparison table can offer a concise and clear way to understand the differences between antibodies and T cells. Here is a table comparing various aspects of both:
| Attribute | Antibodies | T Cells |
|---|---|---|
| Type | Proteins | Cells |
| Primary Function | Neutralize and tag pathogens | Kill infected cells & regulate immunity |
| Produced By | B Cells | Thymus-matured T lymphocytes |
| Targets | Extracellular pathogens | Intracellular pathogens, cancer cells |
| Types | IgG, IgA, IgM, IgD, IgE | Helper, Cytotoxic, Regulatory, Memory |
| Mode of Action | Neutralization, Opsonization, etc. | Direct killing, Coordination, Suppression |
| Memory | Memory B Cells | Memory T Cells |
| Duration | Weeks to months (varies) | Long-term (years; varies) |
| Scope | Broad (various pathogens) | More specific (e.g., virally infected cells) |
| Location | Bloodstream, tissue fluids | Blood, tissues, lymphoid organs |
| Limitations | Cannot target intracellular pathogens | Ineffective against extracellular pathogens |
| Real-world Applications | Vaccines, Diagnostics, Monoclonal therapies | Cancer immunotherapy, Organ transplant management |
This table simplifies complex biological mechanisms for easier comprehension but should provide a general overview of how antibodies and T cells compare and contrast.
Duration and Memory of Antibodies and T Cells
Duration and Memory of Antibodies
- Duration: Once produced, antibodies can circulate in the bloodstream and be present in tissues for varying lengths of time depending on the type of antibody and the nature of the immune response. For example, IgG antibodies can last for weeks to months, offering prolonged protection.
- Memory B Cells: When B cells encounter an antigen and receive appropriate signals, some differentiate into memory B cells. These cells can persist for years or even decades, providing long-term immunity. Upon re-exposure to the same antigen, memory B cells can quickly differentiate into plasma cells to produce antibodies, allowing for a faster and more potent immune response.
- Passive Immunity: Antibodies can also be transferred passively (e.g., from mother to child through breast milk), providing temporary immunity without requiring the immune system to produce its own antibodies.
Duration and Memory of T Cells
- Duration: Like antibodies, the lifespan of T cells varies. Some activated T cells can die off once an infection is cleared, but others persist in a resting state.
- Memory T Cells: These are long-lived T cells generated following an infection. Memory T cells remain dormant until they encounter their specific antigen again. Upon re-exposure, they rapidly proliferate and activate, leading to a quicker and more effective immune response.
- Central and Effector Memory T Cells: Memory T cells can further be categorized into central memory and effector memory cells. Central memory T cells are long-lived and reside in lymphoid tissues, ready to stimulate the immune system when encountering the antigen again. Effector memory T cells are more likely to stay in non-lymphoid tissues and provide immediate protection upon re-exposure to the antigen.
- Cross-Reactivity: In some cases, T cells generated against one pathogen might also offer some level of protection against another related pathogen, although this is generally less specific than the reactivity of memory cells.
Both antibodies and T cells contribute to the body’s memory and long-term immunity, each with its own set of advantages and limitations. This memory aspect is fundamental to the success of vaccination programs and the body’s ability to fight off recurring or similar infections.
Real-world Applications
The understanding of antibodies and T cells has led to a variety of real-world applications that have significantly impacted healthcare, diagnostics, and therapeutics. Here are some key examples:
Real-World Applications of Antibodies
- Vaccines: Many vaccines work by stimulating the production of antibodies specific to a particular pathogen, providing long-lasting immunity.
- Diagnostic Tests: Antibody tests can diagnose infections, allergies, and autoimmune diseases by detecting the presence of specific antibodies in a person’s blood.
- Monoclonal Antibody Therapies: Custom-made antibodies can be designed to target specific proteins, such as in the treatment of cancers and autoimmune diseases.
- Allergy Treatments: IgE antibodies play a role in allergic reactions. Treatments may involve medications that inhibit IgE activity.
- Antivenoms: These are specific antibodies or antibody fragments that can neutralize toxins, such as those from snake or spider bites.
- Passive Immunity: Transfusion of antibodies, as in the administration of convalescent plasma, can provide short-term protection against infections.
Real-World Applications of T Cells
- Cancer Immunotherapy: Techniques like CAR-T cell therapy modify a patient’s own T cells to target cancer cells more effectively.
- Vaccines: Some vaccines aim to stimulate not just an antibody response but also a T cell response for more comprehensive protection.
- HIV Treatment: Research in using T cells is ongoing to improve treatments for HIV, which primarily attacks CD4+ helper T cells.
- Organ Transplant: Understanding T cell responses helps in the management of organ transplant rejection, allowing for better immunosuppressive treatments.
- Autoimmune Disease: Therapies that modulate T cell activity are being developed to treat autoimmune conditions like multiple sclerosis and type 1 diabetes.
- Infectious Diseases: In diseases like tuberculosis, where the bacteria reside within cells, T cell-based therapies and vaccines are under investigation.
By understanding the roles and limitations of antibodies and T cells, researchers and medical professionals are better equipped to develop effective therapies, vaccines, and diagnostic tools. These real-world applications have profound implications for improving health outcomes in a range of diseases and conditions.
Limitations of Antibodies and T Cells
Understanding the limitations of antibodies and T cells is important for gaining a comprehensive view of how the immune system works, as well as for developing strategies to overcome these limitations in medical treatments and interventions.
Here are some of the limitations of antibodies and T cells:
Limitations of Antibodies
- Inability to Target Intracellular Pathogens: Antibodies generally work in the bloodstream and extracellular fluid. They are less effective against pathogens that reside inside cells, like certain viruses and bacteria.
- Antigenic Variation: Some pathogens can change their surface antigens, making it difficult for pre-existing antibodies to recognize and target them.
- Specificity: Antibodies are highly specific to particular antigens. While this is generally advantageous, it also means that antibodies to one pathogen generally can’t fight off another unrelated pathogen.
- Neutralizing vs. Non-Neutralizing: Not all antibodies are equally effective. Some might bind to a pathogen but not neutralize it, allowing the pathogen to continue its activity.
- Dependence on Immune System Activation: Antibody production requires time and activation of the adaptive immune system, which means they are not available immediately upon infection.
- Resource-Intensive Production: Generating antibodies, particularly in therapeutic contexts like monoclonal antibody treatments, is time-consuming and expensive.
Limitations of T Cells
- Limited Scope: T cells are generally ineffective against extracellular pathogens like some bacteria and parasites that antibodies can target more effectively.
- Autoimmune Reactions: In some cases, T cells may mistakenly target the body’s own cells, leading to autoimmune diseases.
- Cancer Evasion: Some cancer cells have mechanisms to evade detection and destruction by T cells, making them less effective in targeting these cells.
- Tolerance Issues: Regulatory T cells can sometimes suppress immune responses too much, leading to higher susceptibility to infections.
- Cellular Resource Intensive: T cell responses also require time and cellular resources to develop. Initial activation, proliferation, and differentiation are energy-consuming processes.
- Exhaustion: In chronic infections or cancers, T cells can become exhausted, losing their ability to effectively combat the pathogen or tumor.
Understanding these limitations can guide research and treatment strategies, from vaccine development to the treatment of autoimmune diseases and cancer. Despite these limitations, antibodies and T cells are incredibly effective in managing a vast array of pathogens and conditions, serving as the cornerstone of adaptive immunity.
The Future of Antibodies and T Cells in Medicine
The future of antibodies and T cells in medicine looks promising, thanks in large part to advances in biotechnology, immunology, and precision medicine. As our understanding of these components of the immune system deepens, we can expect several trends and innovations to shape their role in healthcare.
Future of Antibodies in Medicine
- Advanced Monoclonal Antibodies: Continued development of highly specific and effective monoclonal antibodies will likely revolutionize the treatment of cancers, autoimmune diseases, and even neurodegenerative disorders like Alzheimer’s.
- Bispecific Antibodies: These are engineered antibodies that can target two different antigens simultaneously. They offer the possibility of more effective treatments for complex diseases.
- Antibody-Drug Conjugates: Combining antibodies with chemotherapy drugs can specifically target cancer cells, reducing damage to healthy tissues.
- Rapid Diagnostic Technologies: Portable and quick antibody tests may become increasingly available for immediate diagnosis of diseases, potentially even at home.
- Vaccine Development: Advances in understanding how antibodies work could lead to more effective vaccines, including universal vaccines for rapidly mutating viruses like influenza and potentially even HIV.
- Antibody Engineering for Longevity: Efforts are being made to engineer antibodies with longer half-lives, reducing the frequency of drug administration.
Future of T Cells in Medicine
- CAR-T Therapies: The success of CAR-T in treating certain types of cancer is likely just the tip of the iceberg, with research ongoing for treating other cancers and even some chronic infections.
- T-Cell Vaccines: Traditional vaccines focus on antibody responses, but vaccines that elicit strong T cell responses could offer better protection against diseases like tuberculosis and malaria.
- Autoimmunity and Allergies: Better understanding of regulatory T cells could provide new treatment avenues for autoimmune diseases and severe allergies.
- T-Cell Therapies for Infectious Diseases: There is ongoing research to harness T cells for the treatment of chronic viral infections like HIV and hepatitis.
- Tissue Engineering: Understanding how T cells interact with tissues could be essential in the field of regenerative medicine and organ transplantation.
- T Cell Longevity: Research into prolonging the lifespan and efficacy of therapeutic T cells is ongoing, aiming for more enduring treatments.
Combined Future Applications
- Multi-Modal Therapies: Combining antibody and T cell therapies could offer synergistic effects for treating complex diseases.
- Personalized Medicine: As diagnostic techniques improve, treatments could be tailored more precisely to individual patients’ immune profiles.
- AI and Machine Learning: These technologies could help in discovering new antibody and T cell therapies more rapidly, as well as in understanding complex immune interactions.
- Global Health: Advances in antibody and T cell science could play a significant role in managing global health challenges, including emerging infectious diseases and antibiotic resistance.
- Ethical and Safety Considerations: As with all medical advances, ethical considerations, including equitable access and long-term safety, will be important factors shaping the future of antibody and T cell therapies.
The future of antibodies and T cells in medicine holds immense promise. As our understanding continues to grow, these components of the immune system will likely play an increasingly pivotal role in treating a wide range of diseases and conditions.
Conclusion
Antibodies and T cells are integral components of the adaptive immune system, each with unique functions, capabilities, and limitations. While antibodies excel in neutralizing extracellular pathogens and toxins, T cells are specialized in targeting intracellular threats and regulating immune responses.
Advances in medical science are harnessing the potential of both for diagnostics, treatments, and vaccines, promising a future where personalized, effective therapies are more accessible. Despite their individual limitations, their combined roles provide a robust defense mechanism, making them invaluable tools in the ongoing quest to understand and combat disease.