Granuloma and Keloid represent two distinct types of skin and tissue reactions that the body can produce in response to various triggers. A granuloma forms as a chronic inflammatory reaction, often resulting from the body’s attempt to wall off foreign substances or persistent irritants, leading to the creation of small, firm nodules comprised primarily of immune cells.
On the other hand, a keloid is the result of an overzealous healing process, wherein an overgrowth of dense fibrous tissue extends beyond the borders of an original skin injury. This response can lead to raised, shiny, and often darkened scars that can be both a cosmetic and functional concern for individuals. Both conditions, although different in their origins and presentations, underscore the complexity of the body’s repair and defense mechanisms.
What is Granuloma?
A Granuloma is a localized, nodular inflammatory reaction composed primarily of macrophages, often accompanied by other immune cells such as lymphocytes and giant cells, that forms in response to persistent, non-degradable substances or certain infections. This reaction serves to wall off and contain the foreign material or infectious agent that the body is unable to easily eliminate.

Causes of Granuloma
Granulomas form as a response to a variety of triggers. The body creates these nodular structures in an attempt to isolate and contain substances or pathogens that it cannot easily eliminate. Here are the primary causes of granulomas:
- Foreign Bodies: The presence of non-degradable materials, such as splinters, suture materials, or silica, can prompt the body to form a granuloma around the object to isolate it from surrounding tissue.
- Infections: Certain microorganisms can cause granulomatous reactions. Notable infectious agents include:
- Mycobacteria: Such as Mycobacterium tuberculosis (causing tuberculosis) and Mycobacterium leprae (causing leprosy).
- Fungi: Some fungal infections, like histoplasmosis, coccidioidomycosis, and blastomycosis, can lead to granuloma formation.
- Parasites: Some parasitic infections can result in granulomas, particularly if the parasites or their eggs become lodged in tissue.
- Non-Infectious Inflammatory Conditions: Several non-infectious diseases can lead to granuloma formation, including:
- Sarcoidosis: An idiopathic disease where granulomas commonly form in the lungs, skin, and lymph nodes.
- Crohn’s Disease: A type of inflammatory bowel disease, where granulomas can form in the intestinal wall.
- Wegener’s Granulomatosis (now called Granulomatosis with Polyangiitis): An autoimmune condition affecting the blood vessels.
- Unknown Causes: In some cases, the exact cause of granuloma formation remains unknown. For instance, the underlying triggers for conditions like sarcoidosis are still not fully understood.
- Chemical Agents: Some chemicals, when introduced to the body, can lead to granuloma formation. For instance, certain dermal fillers used in cosmetic procedures can sometimes cause granulomatous reactions.
- Vaccines: Rarely, some vaccines can lead to granuloma formation at the injection site.
While granulomas are generally a protective mechanism, their formation can sometimes result in tissue damage or interfere with the normal function of organs, depending on their size, location, and number. Proper diagnosis and treatment are essential to manage the underlying cause effectively.
Symptoms of Granuloma
The symptoms of granulomas can vary widely based on their cause, location, size, and the specific organs or tissues involved. In many cases, granulomas may not cause any symptoms, especially if they are small and located in non-critical areas. When symptoms do occur, they can include:
- Skin Granulomas:
- Raised, reddish or pink nodules or bumps.
- Potential tenderness or itchiness.
- Possible ulceration or discharge, especially in infectious granulomas.
- Lung Granulomas (e.g., due to sarcoidosis or tuberculosis):
- Persistent cough.
- Shortness of breath.
- Chest pain.
- Wheezing.
- Lymph Node Granulomas:
- Swollen lymph nodes.
- Possible tenderness.
- Liver and Spleen Granulomas:
- Abdominal pain or discomfort.
- Fatigue or malaise.
- Enlargement of the liver or spleen (hepatosplenomegaly).
- Granulomas in Eyes:
- Redness.
- Pain or discomfort.
- Blurred vision or vision loss.
- Sensitivity to light (photophobia).
- Granulomas in the Nervous System:
- Neurological symptoms, depending on the affected area, such as seizures, numbness, weakness, or cognitive changes.
- General Symptoms (especially in systemic conditions like sarcoidosis):
- Fatigue.
- Fever or night sweats.
- Weight loss.
- Joint pain or stiffness.
- Digestive Tract Granulomas (e.g., due to Crohn’s disease):
- Abdominal pain.
- Diarrhea or constipation.
- Blood in stool.
- Nausea or vomiting.
Remember, the manifestation of these symptoms can be subtle or more pronounced, depending on the underlying cause and the progression of the disease or condition that’s prompting granuloma formation. If someone suspects they have a granuloma or is experiencing unexplained symptoms, they should seek medical evaluation.
What is Keloid?
A Keloid is an overgrowth of dense fibrous tissue that forms at the site of a skin injury, such as a surgical incision, wound, or piercing. It results from an excessive healing response and extends beyond the borders of the original injury, leading to raised, often shiny and darkened scars that can be both cosmetically and functionally concerning. Keloids can sometimes be painful or itchy and may continue to grow over time. They are more common in individuals with darker skin and often have a genetic component.

Causes of Keloid
Keloids are the result of an overactive scarring process where the body produces an excessive amount of collagen at the site of a healed skin injury. The causes and risk factors associated with keloid formation include:
- Skin Injuries: Almost any injury to the skin can lead to keloid formation in predisposed individuals. Common triggers include:
- Surgical incisions: Scars from surgeries can develop into keloids.
- Traumatic wounds: Accidental cuts, burns, or abrasions.
- Piercings: Especially ear piercings, but any body piercing can be a potential site.
- Acne, chickenpox, and smallpox scars: Any skin condition that can cause scarring might lead to keloids.
- Vaccination sites: Rarely, keloids may form at the injection site.
- Genetic Predisposition: There’s evidence suggesting a genetic component to keloid formation. Individuals with a family history of keloids are more likely to develop them.
- Hormonal Influences: Changes in hormone levels might influence keloid development and growth. For instance, keloids can sometimes appear or grow during pregnancy or puberty.
- Skin Type: While anyone can develop keloids, they are more common in people with darker skin tones. Individuals of African, Hispanic, and Asian descent have a higher risk of keloid formation.
- Age: While keloids can occur at any age, they are more common in younger individuals and less frequent in the elderly and very young children.
- Location on the Body: Certain areas of the body, such as the chest, back, shoulders, and earlobes, are more prone to keloid formation compared to others.
- Tension on Wound: Wounds under high tension or those that are pulled apart while healing (like over a joint) may have a higher risk of keloid formation.
Everyone who gets a skin injury will develop a keloid, and it’s not entirely clear why some people are more prone to developing them than others. Preventative measures, early intervention, and certain treatments can help manage and reduce the appearance and discomfort of keloids. If someone suspects they’re developing a keloid or has concerns about scarring, they should consult a dermatologist or medical professional.
Symptoms of Keloid
Keloids are primarily a cosmetic concern, but they can also cause a range of symptoms and discomfort. Here are the primary symptoms and characteristics of keloids:
- Appearance:
- Raised and firm scar tissue that continues to grow over time.
- Often shiny or glossy on the surface.
- Typically darker (hyperpigmented) than the surrounding skin, sometimes appearing reddish, pink, or purple initially and becoming brown or tan over time.
- Texture:
- Keloids may feel hard and rubbery to touch.
- They can be irregular in shape and may have a smooth or uneven surface.
- Size and Growth:
- Varies significantly. Some can be tiny and localized, while others grow much larger than the original injury.
- They might continue to grow slowly for weeks, months, or even years.
- Location:
- Most commonly found on the chest, shoulders, earlobes, upper arms, and back. However, they can form anywhere on the body.
- Pain and Discomfort:
- Keloids can be itchy.
- They may cause pain or tenderness, especially when they’re growing.
- Some people experience a burning sensation in the keloid.
- Range of Motion:
- If located near a joint or on a finger, a keloid can potentially limit the range of motion due to its size or tightness.
- Recurrent Inflammation:
- Keloids can occasionally become recurrently inflamed or red.
- Psychological Impact:
- While not a physical symptom, it’s worth noting that keloids can have a significant psychological impact on some individuals due to their appearance, leading to reduced self-esteem or self-consciousness.
It’s essential to differentiate keloids from hypertrophic scars. While both involve an overproduction of tissue at the site of a wound, hypertrophic scars don’t grow beyond the boundaries of the original injury and typically improve over time, whereas keloids expand beyond the initial injury and may not improve without intervention. If someone suspects they have a keloid or is concerned about their scars’ appearance or discomfort, they should consult a dermatologist or medical professional for evaluation and potential treatment options.
Comparison table of Granuloma and Keloid
Here’s a comparison table highlighting the differences between a granuloma and a keloid:
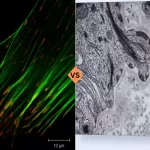
| Feature | Granuloma | Keloid |
|---|---|---|
| Definition | A localized, nodular inflammatory reaction, composed mainly of macrophages, formed in response to persistent foreign substances or infections. | An overgrowth of dense fibrous tissue resulting from an excessive healing response at the site of a skin injury. |
| Cause | – Foreign bodies (e.g., splinters)
– Certain infections (e.g., tuberculosis) – Inflammatory conditions (e.g., sarcoidosis) |
– Surgical incisions
– Wounds – Piercings – Burns |
| Appearance | Small, firm, reddish or pink nodule | Raised, shiny, darkened scar extending beyond the original injury’s borders |
| Histology | Central accumulation of macrophages, often with giant cells and a peripheral halo of lymphocytes. | Thick bundles of collagen with an abundance of fibroblasts. |
| Pain or Itchiness | May or may not be painful | Often itchy or painful |
| Growth Pattern | Typically remains localized | Can continue to grow over time |
| Genetic Predisposition | Depends on the type (e.g., sarcoidosis has some genetic factors) | Yes, especially common in individuals with darker skin tones |
| Treatment | Depends on the cause; may involve antimicrobials, anti-inflammatories, or removal of the foreign body | Corticosteroid injections, laser therapy, surgical removal, silicone sheets or gels |
This table provides a clear distinction between the two conditions, helping to understand their nature, origin, and characteristics.
Treatment Options for Granuloma and Keloid
Both granulomas and keloids present unique challenges in terms of treatment due to their distinct underlying causes and manifestations. Let’s examine the treatment options for each:
Granuloma Treatment Options
- Observation: Many granulomas, especially those without symptoms, may not require immediate treatment and can be observed for changes over time.
- Antimicrobial Therapy: If an infectious agent (e.g., tuberculosis) causes the granuloma, antimicrobial medications specific to that infection may be prescribed.
- Corticosteroids: These can be administered locally or systemically to reduce inflammation.
- Other Immunosuppressive Drugs: In cases of granulomatous conditions like sarcoidosis, drugs like methotrexate or azathioprine might be used to suppress the immune response.
- Surgical Removal: In cases where the granuloma causes discomfort, obstruction, or cosmetic concerns, surgical excision might be considered.
- Cryotherapy: Freezing the granuloma can sometimes be effective, especially for smaller lesions.
Keloid Treatment Options
- Corticosteroid Injections:
- Administered directly into the keloid tissue, these injections help reduce inflammation, flatten the keloid, and alleviate symptoms like itchiness or pain. Several sessions are typically needed.
- Surgical Excision:
- Removing the keloid surgically can be an option. However, there’s a risk that a new keloid will form in the same place, sometimes even larger than the original. Combining surgery with other treatments (like corticosteroid injections or radiation) can reduce the recurrence risk.
- Laser Therapy:
- Lasers can be used to reduce the redness of keloids and improve their appearance. Pulsed dye lasers are commonly used for this purpose.
- Cryotherapy:
- Freezing the keloid with liquid nitrogen can flatten the lesion. This method is usually employed for smaller keloids.
- Silicone Gel Sheets or Ointments:
- Regular application can help soften and flatten keloids, potentially reducing their appearance and discomfort.
- Radiation:
- Post-surgical radiation can be effective in preventing the recurrence of keloids.
- Pressure Therapy:
- Wearing a pressure garment or bandage over the keloid can help reduce its size. This is more commonly used for large keloids or those in areas like the chest.
- 5-Fluorouracil (5-FU) Injections:
- This chemotherapy drug can be injected into keloids to inhibit their growth.
- Interferon Therapy:
- Injections of interferon can help reduce the size of keloids, though the research on its effectiveness is ongoing.
It’s crucial to consult with a dermatologist or appropriate medical specialist when considering treatments for granulomas or keloids. They can provide guidance tailored to the individual’s specific condition, needs, and health history.
Prevention Tips of Granuloma and Keloid
Preventing the formation of granulomas and keloids is sometimes more effective than treating them after they’ve formed. Here are some prevention tips for both conditions:
Granuloma Prevention:
- Avoid Foreign Bodies:
- Be careful when handling sharp objects to prevent splinters or other foreign bodies from getting embedded in the skin.
- Ensure that any surgical sutures or medical implants used are of good quality and suitable for your body.
- Vaccination:
- Stay updated with recommended vaccines, especially for diseases known to cause granulomas like tuberculosis.
- Good Hygiene and Wound Care:
- Clean and disinfect wounds promptly to reduce the risk of infection, which can lead to granuloma formation.
- Protective Measures:
- Use protective equipment in environments where you’re exposed to potential granuloma-causing agents, such as certain chemicals or dust.
Keloid Prevention:
- Injury Care:
- Promptly and properly treat any skin injuries. Clean, disinfect, and keep wounds moist to encourage healing without excessive scar formation.
- Avoid Elective Procedures:
- If you’re prone to keloids, reconsider elective procedures like piercings or tattoos.
- Pressure Therapy:
- After undergoing surgery or experiencing a wound, consider using silicone gel sheets or pressure dressings, which can reduce the risk of keloid formation.
- Sun Protection:
- Protect scars from the sun as ultraviolet (UV) rays can darken them, making them more noticeable. Darkened scars can also be more prone to keloid formation.
- Corticosteroid Injections:
- If you’re undergoing surgery and have a history of keloids, discuss with your doctor about getting preventive corticosteroid injections at the site of the surgical wound.
- Limit Skin Tension:
- In surgeries or wound closures, techniques that reduce skin tension can help in preventing keloid formation.
- Inform Medical Professionals:
- Always inform healthcare providers about your history of keloids, especially if you’re undergoing a surgical procedure.
Both granulomas and keloids are complex conditions influenced by various factors, including genetics. While prevention methods can be effective, they might not guarantee that you won’t develop these conditions. Regular check-ups and consultations with dermatologists or appropriate specialists can help in early detection and management.
Conclusion
Granulomas and keloids are both responses of the body’s skin and tissue to injuries, infections, or other stimuli, but they have distinct causes and manifestations. Granulomas form due to chronic inflammation, often triggered by infections, foreign substances, or other underlying diseases, and they represent the body’s attempt to isolate and contain the offending agent. Keloids, on the other hand, arise from an overzealous healing process where excess collagen accumulates, leading to raised scars that extend beyond the initial injury site.
Both conditions can present aesthetic and symptomatic concerns for individuals. Though prevention is key, several treatments are available for those affected, ranging from medical interventions to surgical options. Consulting with healthcare professionals ensures appropriate care and management tailored to individual needs.