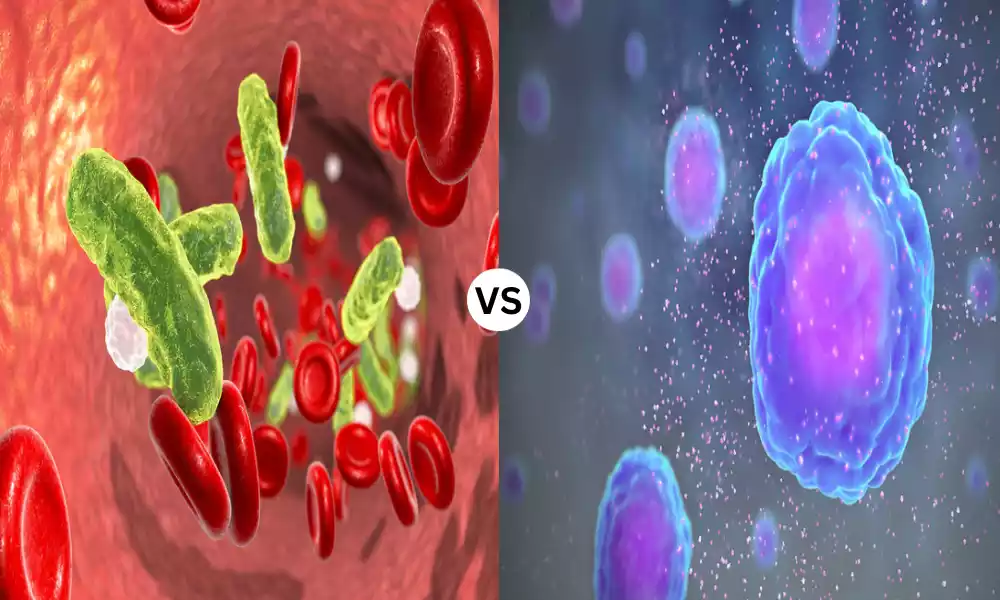
Sepsis and Cytokine Storm are both severe, life-threatening conditions related to the body’s response to pathogens and other triggers, yet they arise from different mechanisms and have distinct presentations. Sepsis is typically triggered by a severe infection, causing the body to respond with a cascade of inflammatory reactions, leading to organ dysfunction, and, potentially, death. It is mainly characterized by the presence of fever, confusion, rapid heartbeat, rapid breathing, and low blood pressure.
On the other hand, a cytokine storm is characterized by an excessive and uncontrolled release of pro-inflammatory cytokines, which can be triggered by various factors including infections, certain drugs, and autoimmune conditions. This overwhelming immune response can lead to widespread inflammation and multi-organ failure. Understanding the distinction between sepsis and cytokine storm is crucial for clinicians to diagnose accurately and administer appropriate, life-saving interventions.
What is Sepsis?
Sepsis is a potentially life-threatening condition resulting from the body’s extreme response to an infection. Instead of localizing a response to a specific area, the body responds with a systemic inflammation that can lead to tissue damage, organ failure, and death. Sepsis arises when the chemicals released into the bloodstream to combat an infection trigger widespread inflammation.

This can lead to a cascade of changes that cause damage to organ systems, causing them to fail. If sepsis progresses to septic shock, blood pressure drops dramatically, further increasing the risk of potential organ failure and death. Early detection and appropriate treatment are crucial, as the condition can rapidly deteriorate. Symptoms of sepsis can include fever, difficulty breathing, low blood pressure, fast heart rate, and mental confusion.
Symptoms of Sepsis
Sepsis can manifest with a variety of symptoms, which can range from mild to severe. Recognizing these symptoms early is crucial, as rapid intervention can be lifesaving. Common symptoms of sepsis include:
- Fever or, conversely, hypothermia (a body temperature below normal).
- Increased heart rate (tachycardia).
- Increased respiratory rate (tachypnea).
- Low blood pressure (hypotension), especially if sepsis progresses to septic shock.
- Confusion or altered mental status.
- Edema (swelling).
- High blood glucose without a history of diabetes.
- Decreased urine output.
- Shortness of breath.
- Skin manifestations:
- Cold, clammy, or pale skin.
- Cyanosis (bluish discoloration of the skin and mucous membranes).
- Mottled or discolored skin.
- Nausea or vomiting.
- Diarrhea.
- Chills due to a sudden fever.
- Severe muscle pain.
- Abdominal pain.
- Decreased platelet count, leading to a potential for increased bleeding or bruising.
The symptoms can vary depending on the source of the infection causing sepsis, the patient’s age, underlying health conditions, and other factors. For instance, older adults might not present with the typical symptoms but may display confusion primarily. As the condition worsens, organs can begin to fail, leading to symptoms related to that organ’s dysfunction. Because sepsis can progress rapidly, immediate medical attention is essential when symptoms are observed.
Causes and Risk Factors
Sepsis is caused by the body’s overwhelming and life-threatening response to an infection. It can be triggered by a wide range of infections, but some of the most common include:
- Bacterial Infections: These are the most common culprits. Common bacterial agents include Streptococcus, Escherichia coli (E. coli), and Staphylococcus aureus.
- Viral Infections: Such as respiratory illnesses (e.g., COVID-19) or viral gastroenteritis.
- Fungal Infections: Especially in people with compromised immune systems. Examples include candidiasis or aspergillosis.
- Parasitic Infections: Less common but can include conditions like malaria.
While any type of infection, from pneumonia to a urinary tract infection, can lead to sepsis, the most likely varieties include:
- Pneumonia
- Abdominal infections (e.g., appendicitis, peritonitis)
- Kidney infections (pyelonephritis)
- Bloodstream infections (bacteremia)
Risk Factors for Sepsis
While sepsis can affect anyone, certain groups of people are at a higher risk. The primary risk factors include:
- Age: Infants and elderly individuals are more susceptible.
- Compromised Immune System: This can be due to conditions like HIV/AIDS, cancer treatments, use of immunosuppressive medications, and other diseases that weaken the immune system.
- Chronic Illness: Diseases such as diabetes, kidney disease, lung disease, and cancer can increase the risk.
- Hospitalization: Especially if the patient is in an intensive care unit (ICU). Invasive procedures or devices, like ventilators or catheters, can introduce pathogens.
- Previous History of Sepsis: Having had sepsis once can elevate the risk of future occurrences.
- Wounds or Injuries: Especially severe ones like burns or large wounds.
- Recent Surgery or Medical Procedures.
- Absence of Vaccination: Not getting vaccinated increases the risk of certain infections, which can then potentially lead to sepsis.
Understanding these risk factors is crucial for prevention and early detection of sepsis, especially in vulnerable populations.
What is Cytokine Storm?
A cytokine storm, also known as a cytokine release syndrome (CRS), refers to a severe immune reaction where the body releases an excessive number of cytokines into the bloodstream too quickly. Cytokines are small proteins that play vital roles in regulating the immune response, promoting inflammation, and mediating cell-to-cell communication.
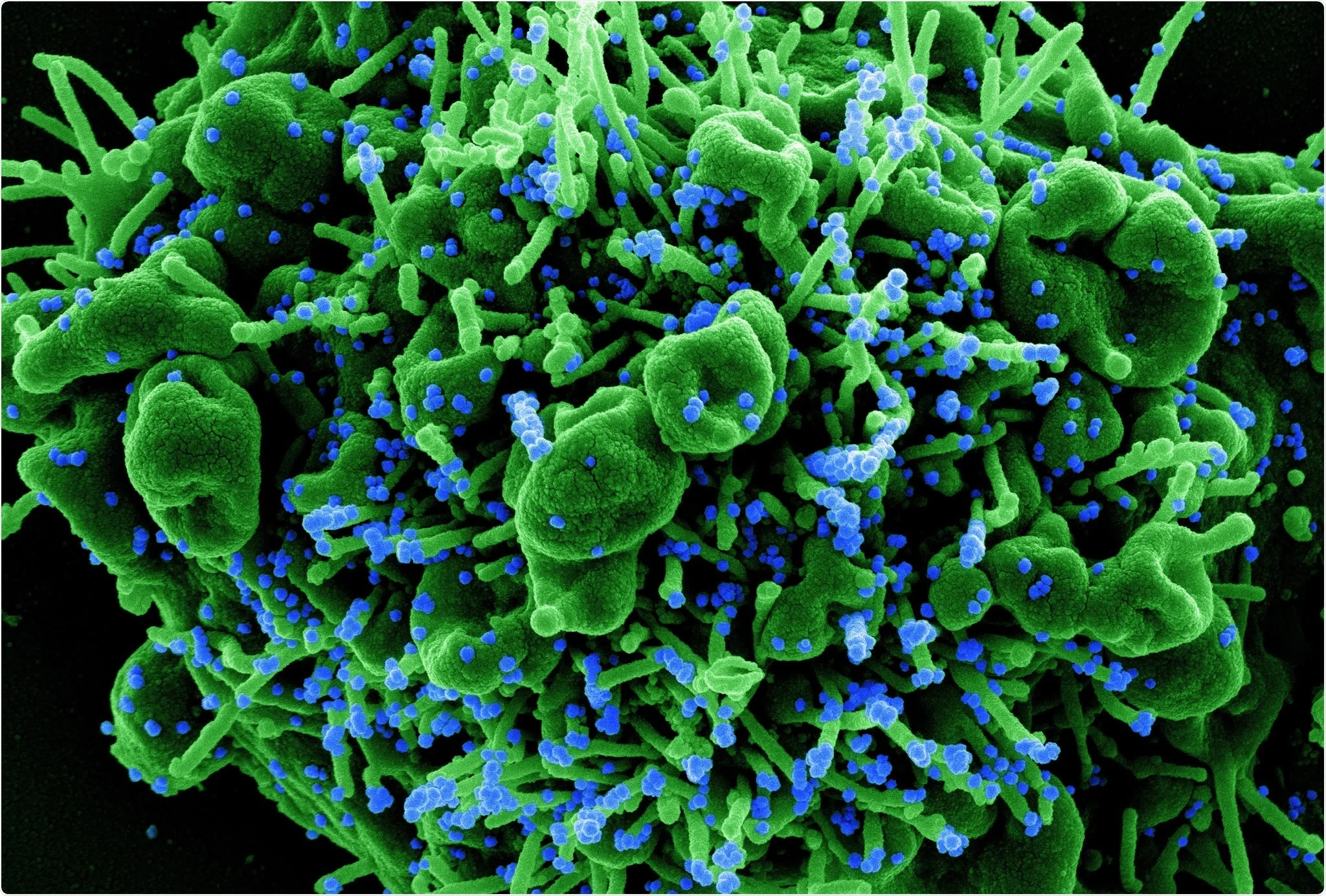
In a cytokine storm, the overwhelming release of these proteins can result in hyperinflammation, potentially leading to serious complications or even death. Instead of precisely targeting the invading pathogens or damaged cells, the immune system goes into overdrive, attacking healthy tissues and organs. This hyperactive immune response can lead to a range of symptoms, including high fever, swelling, redness, extreme fatigue, and nausea. If left untreated, it can cause organ failure and be fatal.
Cytokine storms have been associated with various conditions and diseases, including certain infections like the H5N1 influenza and COVID-19, as well as with some treatments, such as CAR T-cell therapy for cancer. Understanding and managing cytokine storms is critical, especially in conditions where they contribute significantly to morbidity and mortality.
Symptoms of Cytokine Storm
The symptoms of a cytokine storm arise from the extreme inflammatory response triggered by the excessive release of cytokines. These symptoms can vary in severity and may affect multiple organ systems. The following are common symptoms and clinical manifestations associated with a cytokine storm:
- Fever: Often high and persistent.
- Fatigue: Extreme tiredness and weakness.
- Difficulty Breathing: This can range from shortness of breath to acute respiratory distress syndrome (ARDS), which may require mechanical ventilation.
- Reduced Blood Oxygen Levels (hypoxia).
- Tachycardia: Elevated heart rate.
- Hypotension: Reduced blood pressure, which can lead to shock.
- Gastrointestinal Symptoms:
- Nausea
- Vomiting
- Diarrhea
- Rash or Skin Discoloration.
- Joint Pain.
- Organ Dysfunction:
- Liver: Elevated liver enzymes, jaundice.
- Kidney: Reduced urine output, elevated creatinine.
- Heart: Myocarditis, arrhythmias.
- Lungs: Pulmonary edema, ARDS.
- Brain: Confusion, seizures, or even coma.
- Hemophagocytic Lymphohistiocytosis (HLH): A condition where the body makes too many activated immune cells, leading to multi-organ damage.
- Coagulation Abnormalities: This can manifest as disseminated intravascular coagulation (DIC), leading to both excessive clotting and excessive bleeding.
- Elevated Levels of Inflammatory Markers: Such as ferritin, C-reactive protein (CRP), and D-dimer, which are typically detected through blood tests.
- Lymphadenopathy: Swelling of the lymph nodes.
- Sore Throat or Cough.
It’s essential to recognize that the symptoms of a cytokine storm can overlap with the symptoms of the underlying condition triggering it, like an infection or an autoimmune reaction. As cytokine storm can progress rapidly and be life-threatening, early detection and appropriate treatment are crucial.
Causes and Risk Factors Cytokine Storm
A cytokine storm can be triggered by various factors and conditions, primarily resulting from an overreaction of the immune system. The primary causes include:
- Infections:
- Viral: Such as influenza (notably H5N1), COVID-19, and Epstein-Barr virus (EBV).
- Bacterial: Severe bacterial infections can also lead to cytokine storm-like reactions.
- Other: Fungal or parasitic infections in some cases.
- Rheumatologic Diseases: Conditions like systemic juvenile idiopathic arthritis or adult-onset Still’s disease can precipitate a cytokine storm.
- Certain Medications and Therapies:
- CAR T-Cell Therapy: Used to treat certain cancers, particularly some types of lymphoma and leukemia.
- Biologic Therapies: Drugs that modify the immune response, such as those targeting specific immune cells or cytokines.
- Malignancies: Some types of cancers, particularly lymphomas or leukemias, can be associated with cytokine release syndromes.
- Genetic Factors: Some inherited conditions, like familial HLH (hemophagocytic lymphohistiocytosis), predispose individuals to cytokine storms.
- Autoimmune and Autoinflammatory Diseases: Conditions like systemic lupus erythematosus (SLE) or macrophage activation syndrome (MAS) can sometimes trigger excessive cytokine release.
Risk Factors for Cytokine Storm
While the direct causes lead to the onset of a cytokine storm, several factors can increase an individual’s risk:
- Pre-existing Immune System Abnormalities: Any condition or treatment that affects the immune system can increase the risk.
- Recent Immune System Activation: Having recently fought off an infection or received a vaccine might temporarily increase susceptibility in specific contexts.
- Age: Both the very young and the elderly can have exaggerated immune responses.
- Presence of Chronic Diseases: Conditions like diabetes, obesity, or chronic respiratory diseases can make individuals more susceptible to severe infections, which in turn can lead to a cytokine storm.
- Genetic Predisposition: Some individuals might have a genetic makeup that makes them more prone to cytokine storms when confronted with triggers.
- Previous Episodes: Individuals who have experienced a cytokine storm before might be at an increased risk of encountering another one.
Understanding the causes and risk factors associated with cytokine storms is vital for prevention, especially in contexts where risks are modifiable or when considering specific therapeutic interventions that might provoke a cytokine release syndrome.
Comparison table of Sepsis and Cytokine Storm
Here’s a comparison table that provides an overview of the key differences between sepsis and cytokine storm:
| Feature | Sepsis | Cytokine Storm |
|---|---|---|
| Definition | A life-threatening response to infection resulting in systemic inflammation, leading to organ dysfunction. | An excessive and uncontrolled release of cytokines, leading to hyperinflammation and potential organ failure. |
| Primary Causes | Most often caused by bacterial infections, but can also be caused by viral, fungal, or parasitic infections. | Various triggers including infections (especially certain viruses), immune therapies, rheumatologic diseases, and some malignancies. |
| Key Symptoms | Fever, confusion, rapid heartbeat, rapid breathing, low blood pressure, potential organ dysfunction. | High fever, fatigue, difficulty breathing, reduced blood oxygen levels, organ dysfunction, elevated levels of inflammatory markers. |
| Underlying Mechanism | The body’s response to a severe infection, leading to a cascade of inflammatory reactions. | Overwhelming immune response with excessive cytokine release, causing the immune system to attack healthy tissues/organs. |
| Risk Groups | Infants, elderly, those with compromised immune systems, chronic illnesses, recent surgery or invasive procedures. | Individuals with pre-existing immune abnormalities, recent immune system activation, certain genetic predispositions, or those undergoing specific immune therapies. |
| Treatment | Broad-spectrum antibiotics (initially), fluids, vasoactive medications, and support for failing organs, e.g., mechanical ventilation for respiratory failure. | Immunosuppressive drugs, corticosteroids, targeted therapies like tocilizumab (for IL-6 inhibition), and support for affected organs. |
| Diagnostic Indicators | Based on clinical symptoms, blood tests showing elevated inflammatory markers, organ dysfunction markers, and potential pathogen identification. | Clinical symptoms, extremely high levels of certain cytokines, and other inflammatory markers in the blood. |
| Potential Complications | Septic shock, multi-organ failure, death. | Multi-organ failure, respiratory failure, coagulation abnormalities, death. |
This table provides a general overview, but it’s important to understand that both sepsis and cytokine storms are complex conditions with varying presentations and overlaps. Clinical judgment and comprehensive evaluation are crucial for accurate diagnosis and management.
Similarities between Sepsis and Cytokine Storm
Sepsis and cytokine storm, while distinct in origin and specific mechanisms, share several similarities in their manifestations and effects on the body. Here are some of the commonalities between the two:
- Systemic Inflammatory Response: Both conditions are characterized by an excessive and widespread inflammatory response in the body.
- Organ Dysfunction: Due to the systemic nature of the inflammation, multiple organ systems can be affected in both sepsis and cytokine storm, potentially leading to organ failure.
- Symptom Overlap: Common symptoms between the two include fever, increased heart rate, increased respiratory rate, confusion, and low blood pressure.
- Life-threatening: Both sepsis and cytokine storm can be rapidly progressive and life-threatening if not recognized and treated promptly.
- Elevated Inflammatory Markers: Blood tests in both conditions often reveal elevated levels of inflammatory markers such as C-reactive protein (CRP), procalcitonin, and others.
- Potential for Respiratory Failure: Both conditions can lead to acute respiratory distress syndrome (ARDS) and the need for mechanical ventilation.
- Treatment Strategies: Management of both conditions may involve ICU care, hemodynamic support, and the use of specific medications to modulate the immune response.
- Potential Triggers: While sepsis is primarily triggered by infections, certain infections (especially viral) can also lead to cytokine storms. For example, COVID-19 can lead to both sepsis and cytokine storm in severely affected patients.
- Coagulation Abnormalities: Both sepsis and cytokine storm can be associated with clotting disorders, leading to complications such as disseminated intravascular coagulation (DIC).
- Shared Risk Groups: Certain populations, such as the elderly, those with compromised immune systems, and those with chronic medical conditions, are at increased risk for both sepsis and cytokine storms.
While there are similarities, it’s essential to differentiate between the two conditions, as they might require different therapeutic approaches. However, understanding the commonalities can aid in early recognition and management.
Treatment Approaches
Treatment approaches for sepsis and cytokine storm differ based on their causes and pathophysiology, but some elements of treatment overlap due to their shared systemic inflammatory nature. Here’s a breakdown:
Sepsis:
- Early Antibiotic Administration: Once sepsis is suspected, broad-spectrum antibiotics are usually started immediately, even before the exact causative agent is identified. Later, antibiotics may be adjusted based on culture results and sensitivities.
- Fluid Resuscitation: Intravenous fluids are given to maintain blood pressure and ensure adequate organ perfusion.
- Vasoactive Medications: Drugs like norepinephrine, dopamine, or epinephrine can be used to raise blood pressure in septic shock when fluids alone are insufficient.
- Organ Support: Depending on the organs affected:
- Respiratory: Mechanical ventilation for patients with respiratory failure.
- Renal: Dialysis or continuous renal replacement therapy for kidney failure.
- Cardiac: Inotropes to support heart function.
- Source Control: Identifying and addressing the primary source of the infection, such as draining an abscess or removing an infected catheter.
- Monitoring and Support: Continuous monitoring in an ICU setting, with blood tests and other diagnostics to track the patient’s progress and adjust treatment as necessary.
Cytokine Storm:
- Immunosuppression: Corticosteroids, like dexamethasone, can be used to suppress the overactive immune response.
- Targeted Therapies:
- Tocilizumab and Sarilumab: These are IL-6 receptor blockers. IL-6 is one of the cytokines elevated in cytokine storms.
- Anakinra: An IL-1 receptor antagonist.
- Supportive Care: Similar to sepsis, patients might require:
- Respiratory: Oxygen therapy or mechanical ventilation.
- Hemodynamic: Fluid resuscitation and vasoactive medications.
- Renal: Dialysis in cases of kidney failure.
- Cytokine Filtration: Devices that can filter excessive cytokines from the blood, although this is more experimental.
- Treatment of the Underlying Cause: For example, if a medication or infection triggered the cytokine storm, it’s vital to address that cause specifically.
- Monitoring and Support: ICU care with regular blood tests to monitor cytokine levels, organ function, and the overall clinical picture.
Overlapping Elements:
- Both conditions necessitate rapid recognition and intervention to prevent mortality.
- ICU care with close monitoring is often required for both conditions.
- Hemodynamic and respiratory support is a cornerstone in managing both sepsis and cytokine storm.
Both sepsis and cytokine storm are severe conditions that require specialized care. Always consult with a healthcare professional when encountering potential cases of either condition.
Conclusion
Sepsis and cytokine storm represent critical, life-threatening medical conditions characterized by systemic inflammatory responses. While sepsis arises primarily from an uncontrolled reaction to infections, cytokine storm stems from an overzealous immune response releasing excessive cytokines. Despite their distinct triggers, they exhibit overlapping clinical manifestations, including multiple organ dysfunction, fever, and elevated inflammatory markers.
The treatment of both conditions demands rapid intervention, with sepsis often requiring antibiotic therapy and source control, and cytokine storm necessitating immunomodulating agents. Early recognition and comprehensive care are imperative to improve outcomes in these severe systemic reactions.