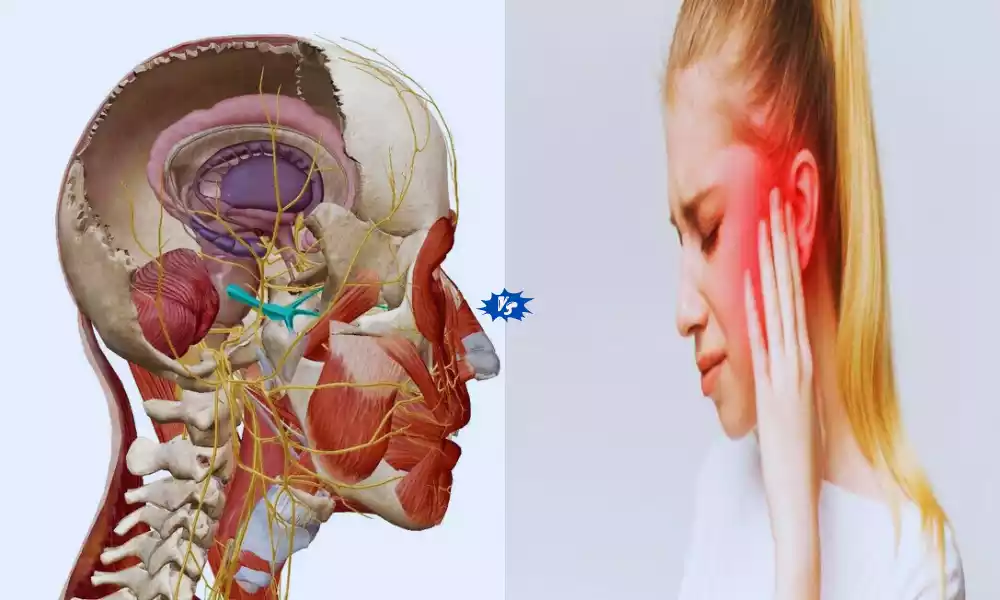
Typical and Atypical Trigeminal Neuralgia is characterized by sudden, excruciating episodes of sharp, electric shock-like pain, often triggered by routine activities like eating or speaking. It is primarily attributed to vascular compression of the trigeminal nerve. Atypical Trigeminal Neuralgia, also known as Type 2 TN, presents with constant, burning, and aching pain, with less distinct trigger points.
Its etiology is often related to factors beyond vascular compression, making it a more complex and challenging condition to diagnose and treat. This differentiation between the two forms of TN is crucial for appropriate management and improved patient outcomes.
What is Typical Trigeminal Neuralgia?
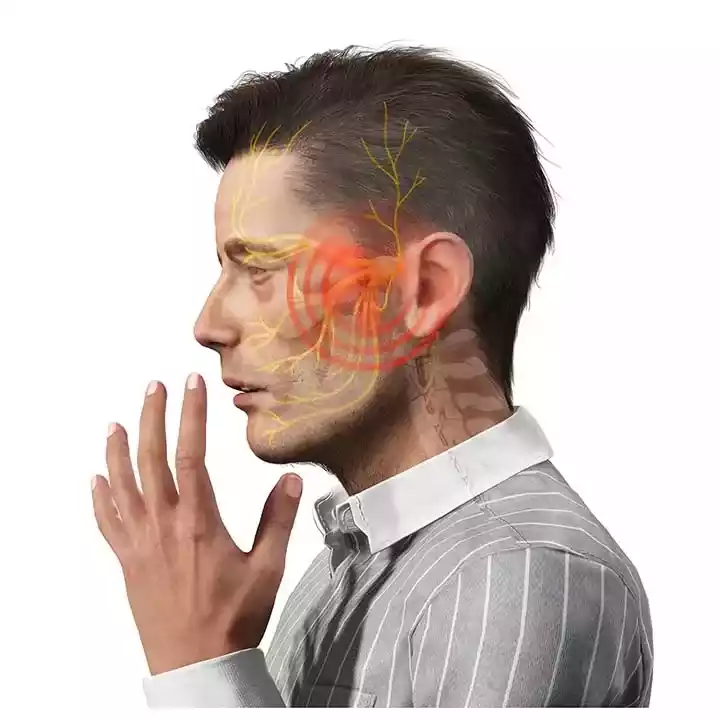
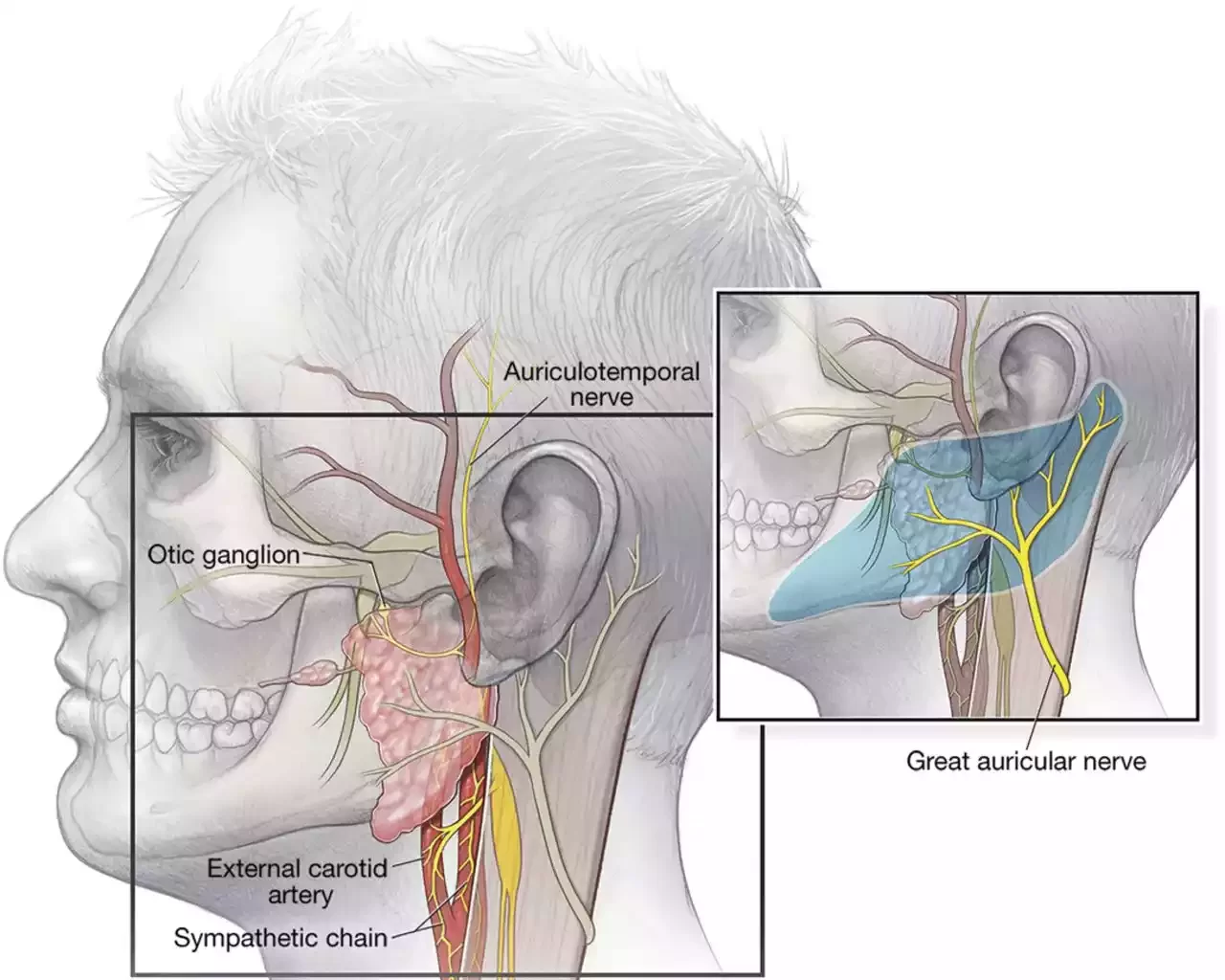
Typical Trigeminal Neuralgia, often referred to as Type 1 TN, is a neurological disorder characterized by recurrent and sudden-onset severe facial pain. This pain is typically described as sharp, stabbing, or electric shock-like and is often triggered by even minor activities such as chewing, talking, or touching the face. It primarily affects the trigeminal nerve, which is responsible for transmitting sensory information from the face to the brain.
Typical TN is usually caused by the compression of the trigeminal nerve by nearby blood vessels, leading to episodes of intense pain in one side of the face. The condition can be excruciating and debilitating, but there are various treatment options available to manage the pain, ranging from medications to surgical interventions like microvascular decompression. Proper diagnosis and management are essential for improving the quality of life for individuals with Typical Trigeminal Neuralgia.
Symptoms
Typical Trigeminal Neuralgia (Type 1 TN) is characterized by specific symptoms that primarily involve sudden and severe facial pain. These symptoms are typically episodic and often follow a specific pattern:
- Sudden, Severe Pain: The hallmark symptom of Typical TN is sudden, intense, and excruciating facial pain. The pain is often described as sharp, stabbing, or electric shock-like in nature.
- Trigger Points: Pain attacks are typically triggered by seemingly harmless and routine activities, such as eating, drinking, speaking, brushing teeth, touching the face, or even exposure to a gentle breeze. These trigger points can vary among individuals and are specific to certain branches of the trigeminal nerve.
- Location: The pain is usually unilateral, affecting one side of the face, and is most commonly felt in the lower part of the face, including the lips, gums, cheek, and jaw. Rarely, it can also involve the forehead and eye area.
- Duration: Pain episodes are typically brief, lasting only a few seconds to a couple of minutes, but they can be intensely painful during this short duration.
- Frequency: TN is characterized by recurrent episodes of pain. Patients may experience multiple episodes daily, with varying levels of intensity and frequency.
- Remission Periods: TN often follows a pattern of remission and recurrence. Some individuals may have periods of relief where they experience little to no pain, followed by sudden and unpredictable flare-ups.
- Absence of Neurological Deficits: Between pain episodes, individuals with TN generally do not exhibit neurological deficits, such as weakness or numbness in the affected facial area.
Typical TN is severe and paroxysmal, making it one of the most painful conditions known. The condition can significantly impact a person’s quality of life, leading to avoidance of trigger activities and social isolation.
If someone experiences symptoms suggestive of Trigeminal Neuralgia, they should seek prompt medical evaluation from a healthcare provider, often a neurologist, to confirm the diagnosis and explore appropriate treatment options to manage the pain.
Cause
Typical Trigeminal Neuralgia (Type 1 TN) is primarily caused by compression or irritation of the trigeminal nerve, which is one of the cranial nerves responsible for transmitting sensory information from the face to the brain. The exact cause of this compression or irritation can vary among individuals, but several factors may contribute to the development of Typical TN:
- Vascular Compression: The most common cause of Typical TN is believed to be vascular compression. In this scenario, blood vessels, often an artery, come into contact with and compress the trigeminal nerve, leading to irritation and the characteristic paroxysms of severe facial pain.
- Arterial Loops: Sometimes, blood vessels near the trigeminal nerve may have abnormal loops or configurations that bring them into close contact with the nerve, resulting in irritation and pain.
- Tumors or Lesions: Rarely, tumors or lesions in the brain or skull base can exert pressure on the trigeminal nerve, causing Typical TN symptoms. These infections may be either benign or malignant in nature.
- Multiple Sclerosis (MS): In some cases, Typical TN may occur as a secondary symptom of multiple sclerosis, an autoimmune disease that affects the central nervous system. MS-related demyelination of the trigeminal nerve can lead to facial pain resembling TN.
- Infection or Inflammation: Inflammation or infection near the trigeminal nerve, such as herpes zoster (shingles), can irritate the nerve and trigger TN-like symptoms.
- Idiopathic: In a minority of cases, the exact cause of Typical Trigeminal Neuralgia remains unknown (idiopathic), even after thorough medical evaluation. These cases are often categorized as essential or primary TN.
Typical TN can vary among individuals, and the condition is typically diagnosed based on clinical symptoms, medical history, and imaging studies like MRI. The primary goal of treatment for Typical TN is to alleviate pain, often through medications or surgical interventions, with the specific approach depending on the individual’s circumstances and the underlying cause if identified.
Diagnosis
Diagnosing Typical Trigeminal Neuralgia (TN) typically involves a comprehensive evaluation by a healthcare provider, often a neurologist or pain specialist, to confirm the diagnosis and rule out other potential causes of facial pain.
Here are the key steps involved in diagnosing Typical Trigeminal Neuralgia:
- Clinical Assessment:
- The healthcare provider will begin by taking a detailed medical history, including asking about the patient’s symptoms, pain characteristics (e.g., location, frequency, triggers), and any relevant medical conditions or medications.
- Physical Examination:
- A physical examination will be conducted to assess the patient’s facial sensation, muscle strength, and reflexes. The healthcare provider may look for signs of trigeminal nerve dysfunction, although these may not be evident between pain episodes.
- Pain Description:
- The patient will be asked to describe the pain, including its quality (e.g., sharp, stabbing, electric shock-like), location (usually in the lower face), and duration of episodes.
- Trigger Points:
- Patients are often asked to identify specific trigger points or activities that provoke their pain. These trigger points are characteristic of TN and help distinguish it from other facial pain disorders.
- Differential Diagnosis:
- Other potential causes of facial pain, such as dental issues, sinusitis, temporomandibular joint disorders, post-herpetic neuralgia, or neuropathic pain conditions, will be considered and ruled out.
- Imaging Studies:
- Magnetic Resonance Imaging (MRI) is a valuable tool for evaluating the trigeminal nerve and surrounding structures. High-resolution MRI can help identify vascular compression or other structural abnormalities that may be causing the neuralgia.
- Response to Medications:
- A positive response to certain medications, such as anticonvulsants like carbamazepine or oxcarbazepine, can provide further support for the diagnosis of Typical TN. These medications are often prescribed as a diagnostic trial to see if they provide pain relief.
- Neurological Evaluation:
- In some cases, additional neurological testing or consultations may be recommended, particularly if there are atypical features or concerns about underlying neurological conditions.
- Documentation:
- Maintaining a detailed pain diary can be helpful for tracking the frequency, duration, and triggers of pain episodes, which can aid in diagnosis and treatment planning.
Once a diagnosis of Typical Trigeminal Neuralgia is confirmed, the healthcare provider can work with the patient to develop an appropriate treatment plan. Treatment options may include medications to manage pain, surgical interventions, or minimally invasive procedures to alleviate the compression of the trigeminal nerve, or a combination of these approaches. Regular follow-up appointments and adjustments to the treatment plan may be necessary to optimize pain management.
What is Atypical Trigeminal Neuralgia?
Atypical Trigeminal Neuralgia, also known as Type 2 TN, is a neurological condition that shares some similarities with the typical form of Trigeminal Neuralgia (TN) but is characterized by distinct differences. In Atypical TN, individuals experience facial pain that is often described as burning, aching, or constant, rather than the sudden, severe, electric shock-like pain seen in typical TN. Unlike typical TN, trigger points for pain are less common or less clearly defined in Atypical TN.
The underlying cause of Atypical TN is typically more complex and may involve factors beyond vascular compression of the trigeminal nerve. This complexity often makes diagnosis and treatment more challenging. Medical professionals may need to rule out other potential causes of facial pain before confirming a diagnosis of Atypical Trigeminal Neuralgia. Treatment options for Atypical TN can include medications like anticonvulsants and antidepressants, nerve blocks, and various surgical interventions like rhizotomy or glycerol injections.
Atypical Trigeminal Neuralgia is a variant of TN characterized by different pain qualities and trigger patterns compared to typical TN, and it often presents diagnostic and therapeutic challenges due to its less defined etiology and symptoms.
Symptoms
Atypical Trigeminal Neuralgia (Type 2 TN) is characterized by symptoms that differ from those of the typical form of Trigeminal Neuralgia (Type 1 TN). The primary symptoms of Atypical Trigeminal Neuralgia include:
- Constant Facial Pain: Unlike the sudden, severe, and intermittent pain of typical TN, Atypical TN is associated with a constant, dull, burning, aching, or throbbing pain in the affected areas of the face.
- Pain Distribution: The pain in Atypical TN can be widespread and may affect multiple areas of the face, not necessarily confined to the branches of the trigeminal nerve.
- Trigger Points Less Common: While trigger points can exist in Atypical TN, they are less common and less well-defined than in typical TN. Activities or triggers that provoke pain may not be as apparent.
- Duration of Pain: The pain experienced in Atypical TN tends to be more persistent and longer-lasting compared to the brief, shock-like episodes of typical TN.
- Less Severe Attacks: While the pain in Atypical TN can be severe, it is generally less intense and paroxysmal (sudden and severe) than the pain seen in typical TN.
- Associated Symptoms: Individuals with Atypical TN may also experience other symptoms, such as tingling, numbness, or a feeling of tightness in the affected facial areas.
- Tenderness: There may be areas of tenderness or sensitivity in the face, although these areas may not correspond to typical trigeminal nerve distributions.
Atypical Trigeminal Neuralgia can be challenging, as these symptoms can overlap with other facial pain disorders or conditions. A thorough clinical evaluation, including medical history and diagnostic tests, is essential to differentiate Atypical TN from other potential causes of facial pain and to determine the most appropriate treatment approach.
Cause
The exact causes of Atypical Trigeminal Neuralgia (Type 2 TN) are not fully understood, and this condition is often considered more complex and less well-defined than typical Trigeminal Neuralgia (Type 1 TN).
Several factors and mechanisms may contribute to the development of Atypical TN:
- Nerve Compression or Damage: While typical TN is primarily associated with vascular compression of the trigeminal nerve, Atypical TN may involve different mechanisms of nerve compression or damage. This can include compression by blood vessels, tumors, or other structures in the vicinity of the trigeminal nerve.
- Multiple Sclerosis (MS): In some cases, Atypical TN may be associated with underlying conditions like multiple sclerosis, an autoimmune disease that affects the central nervous system. MS-related demyelination of the trigeminal nerve can result in facial pain resembling Atypical TN.
- Nerve Irritation or Inflammation: Irritation or inflammation of the trigeminal nerve, often due to various underlying factors, can contribute to Atypical TN. Inflammation of the nerve can lead to persistent facial pain.
- Trauma or Injury: Facial trauma or injury to the trigeminal nerve or surrounding structures may trigger Atypical TN symptoms in some individuals.
- Neurological Disorders: Certain neurological disorders, such as post-herpetic neuralgia (caused by the herpes zoster virus) or other neuropathic pain conditions, can mimic the symptoms of Atypical TN.
- Idiopathic: In some cases, the cause of Atypical TN may remain unclear, and it may be classified as idiopathic, meaning that no specific underlying cause can be identified.
It’s important to emphasize that the diagnosis of Atypical Trigeminal Neuralgia often involves ruling out other potential causes of facial pain and conducting a comprehensive evaluation to determine the most likely contributing factors. Treatment approaches for Atypical TN may vary depending on the underlying cause and individual patient characteristics. Therefore, a thorough evaluation by a healthcare professional, often a neurologist or pain specialist, is essential to develop an appropriate management plan.
Diagnosis
Diagnosing Atypical Trigeminal Neuralgia (Type 2 TN) can be challenging because its symptoms and underlying causes are more complex and less well-defined compared to typical Trigeminal Neuralgia (Type 1 TN). A comprehensive diagnostic process is crucial to rule out other potential causes of facial pain and arrive at an accurate diagnosis.
Here are the steps typically involved in diagnosing Atypical TN:
- Clinical Evaluation:
- A thorough medical history is obtained, including a detailed description of the patient’s pain, its characteristics (constant, burning, aching), and its duration.
- The healthcare provider will inquire about any triggers for the pain and any associated symptoms, such as tingling or numbness.
- A physical examination of the face, head, and neck may be conducted to identify areas of tenderness or sensitivity.
- Neurological Examination:
- A neurological assessment is performed to evaluate sensory function, muscle strength, and reflexes in the face and head.
- The healthcare provider will assess for any signs of trigeminal nerve dysfunction or other neurological abnormalities.
- Imaging Studies:
- Magnetic Resonance Imaging (MRI) is often ordered to visualize the trigeminal nerve and surrounding structures. MRI can help identify any structural abnormalities, such as vascular compression, tumors, or demyelination of the nerve.
- High-resolution imaging techniques and special sequences (e.g., constructive interference in steady state or 3D time-of-flight sequences) may be used to enhance visualization of vascular compression.
- Differential Diagnosis:
- Atypical TN is a diagnosis of exclusion, meaning that other potential causes of facial pain must be ruled out. The healthcare provider will consider conditions like dental issues, sinusitis, temporomandibular joint disorders, post-herpetic neuralgia, and other neuropathic pain disorders.
- Response to Medications:
- A positive response to certain medications, such as anticonvulsants or tricyclic antidepressants, may provide supportive evidence for the diagnosis of Atypical TN. Patients may be prescribed these medications to see if they provide pain relief.
- Consultation with Specialists:
- Depending on the clinical presentation and diagnostic findings, a referral to a neurologist, pain management specialist, or oral and maxillofacial surgeon may be necessary for further evaluation and treatment planning.
- Monitoring and Follow-Up:
- Patients may need ongoing monitoring to assess the response to treatment and the progression of symptoms.
The diagnosis of Atypical Trigeminal Neuralgia often involves a collaborative effort between healthcare providers and may require multiple assessments and tests to arrive at a definitive diagnosis. Given the complexity of the condition, it is essential to consult with experienced healthcare professionals who specialize in the diagnosis and management of trigeminal neuralgia and related facial pain disorders.
Comparison Table of Typical and Atypical Trigeminal Neuralgia
Here’s a comparison table outlining the key differences between Typical and Atypical Trigeminal Neuralgia (TN):
| Characteristic | Typical Trigeminal Neuralgia (Type 1 TN) | Atypical Trigeminal Neuralgia (Type 2 TN) |
|---|---|---|
| Pain Characteristics | Sudden, severe, electric shock-like pain | Constant, burning, aching pain |
| Trigger Points | Common, often triggered by routine activities | Less common, less clearly defined |
| Etiology | Primarily vascular compression of the trigeminal nerve | Complex causes, often beyond vascular compression |
| Diagnosis | Clinical evaluation and imaging (MRI) | Clinical evaluation, exclusion of other causes, imaging (MRI) |
| Treatment Options | Medications (anticonvulsants, tricyclic antidepressants), surgical interventions (microvascular decompression, radiofrequency ablation) | Medications (anticonvulsants, antidepressants), nerve blocks, surgical interventions (rhizotomy, glycerol injection) |
| Prognosis | Generally favorable with treatment, but relapses can occur | Variable, often challenging to manage |
| Pain Quality | Sharp, stabbing, electric shock-like | Burning, aching, constant |
| Trigger Factors | Often triggered by routine facial movements (e.g., eating, speaking) | Trigger points less common or less defined |
| Etiological Complexity | Primarily vascular compression-related | Often multifactorial and less understood |
| Diagnostic Challenges | Relatively straightforward due to characteristic pain and trigger points | Complex, requires ruling out other potential causes of facial pain |
| Management Approach | Focused on relieving pain during episodes and preventing future attacks | Targeting constant pain management and addressing underlying causes |
| Response to Treatment | Typically responsive to medication or surgical interventions | Variable response, may require a combination of therapies |
This table highlights the distinct clinical features, etiological factors, and management considerations that differentiate Typical Trigeminal Neuralgia from Atypical Trigeminal Neuralgia. Each type requires a tailored approach to diagnosis and treatment due to their unique characteristics.
Similarities of Typical and Atypical Trigeminal Neuralgia
While Typical and Atypical Trigeminal Neuralgia (TN) differ in several key aspects, there are also some similarities between the two forms of the condition:
- Facial Pain Impact: Both types of TN can significantly impact an individual’s quality of life due to the severity and chronic nature of facial pain. The pain in both cases can be debilitating and affect daily activities.
- Neurological Basis: Both Typical and Atypical TN are neurological disorders that involve the trigeminal nerve, which is responsible for facial sensation. In both cases, there is a disruption in the normal functioning of this nerve.
- Need for Multidisciplinary Care: Patients with both types of TN often require a multidisciplinary approach to treatment. This may involve collaboration between neurologists, neurosurgeons, pain management specialists, and other healthcare providers to address the complexity of the condition and provide comprehensive care.
- Medications: Medications are a common component of treatment for both types of TN. Anticonvulsants and tricyclic antidepressants, for example, may be prescribed to help manage pain in both Typical and Atypical TN.
- Surgical Interventions: While the specific surgical approaches may differ, both Typical and Atypical TN may require surgical interventions as a treatment option when medications alone are insufficient in providing pain relief.
- Chronic Nature: Both forms of TN are typically chronic conditions, meaning that they persist over time. While the frequency and severity of pain episodes can vary, individuals with either type of TN may experience recurrent pain.
- Emotional Impact: The emotional toll of living with chronic facial pain is a shared experience in both Typical and Atypical TN. Patients with either form may experience anxiety, depression, or other emotional challenges related to their condition.
- Support Groups: Support groups and patient communities can be valuable resources for individuals with both Typical and Atypical TN. These groups provide a safe space to share experiences, discuss ways of coping and receive emotional support.
Despite these similarities, the differences in pain characteristics, trigger points, etiology, and response to treatment necessitate tailored approaches for diagnosis and management of each type of TN. Understanding both the commonalities and distinctions between Typical and Atypical TN is crucial for healthcare providers and patients seeking effective treatment and support.
Treatment for Typical and Atypical Trigeminal Neuralgia
The treatment for both Typical Trigeminal Neuralgia (Type 1 TN) and Atypical Trigeminal Neuralgia (Type 2 TN) involves a combination of medical, surgical, and interventional approaches. The choice of treatment depends on the type of TN, the severity of symptoms, the patient’s overall health, and their response to previous treatments.
Here are the common treatment options for both types of TN:
Medical Management:
- Anticonvulsant Medications: Drugs like carbamazepine (Tegretol), oxcarbazepine (Trileptal), and gabapentin (Neurontin) are often prescribed to control pain in both Typical and Atypical TN.
- Tricyclic Antidepressants: Medications such as amitriptyline (Elavil) and nortriptyline (Pamelor) can help manage pain and are sometimes used as adjuncts to anticonvulsants.
- Baclofen: This muscle relaxant may be prescribed to alleviate muscle spasms that can contribute to pain.
- Opioid Medications: In some cases, opioid medications may be considered for pain management, but their use is generally avoided due to the risk of dependence and other side effects.
- Botulinum Toxin Injections: Injections of botulinum toxin (Botox) may be used to target specific trigger points in the face and provide temporary relief.
Interventional Procedures:
- Nerve Blocks: Local anesthetics or steroids can be injected into the trigeminal nerve or ganglion to provide short-term pain relief. This can be particularly useful in Atypical TN.
- Radiofrequency Ablation: In this procedure, radiofrequency waves are used to damage or destroy the trigeminal nerve fibers, reducing pain signals. This is often considered when medications are ineffective.
Surgical Interventions:
- Microvascular Decompression (MVD): This surgical procedure aims to relieve compression of the trigeminal nerve by repositioning or cushioning the blood vessels causing the pressure. It is a highly effective treatment for Typical TN.
- Rhizotomy: Various forms of rhizotomy, such as glycerol injection, balloon compression, or radiofrequency rhizotomy, involve damaging or disrupting the trigeminal nerve fibers to reduce pain signals.
- Gamma Knife Radiosurgery: This non-invasive procedure uses focused radiation to create lesions on the trigeminal nerve, interrupting pain signals.
- Neurostimulation: Techniques like peripheral nerve stimulation (PNS) or motor cortex stimulation (MCS) involve implanting devices that modulate the nerve activity to alleviate pain.
- Peripheral Nerve Decompression: In some cases, surgeons may explore decompression of peripheral branches of the trigeminal nerve.
It’s crucial to tailor the treatment approach to the specific needs and preferences of the patient, taking into consideration the type of TN and the severity of their symptoms. Additionally, pain management strategies may need to be adjusted over time, and some individuals may benefit from a combination of treatments. A multidisciplinary approach involving neurologists, neurosurgeons, and pain specialists is often essential for comprehensive care and pain management in TN cases.
Summary
Trigeminal Neuralgia (TN) encompasses both Typical (Type 1) and Atypical (Type 2) forms, each characterized by distinct pain profiles, triggers, and underlying causes. While they share the burden of chronic facial pain and require multidisciplinary care, Typical TN is marked by sudden, severe shocks of pain often triggered by routine activities, usually due to vascular compression.
Atypical TN presents with constant, burning pain, is less likely to have clear trigger points, and is associated with a more complex etiology. Recognizing these differences is vital for accurate diagnosis and tailoring treatment approaches to improve the quality of life for individuals living with these challenging neurological conditions.