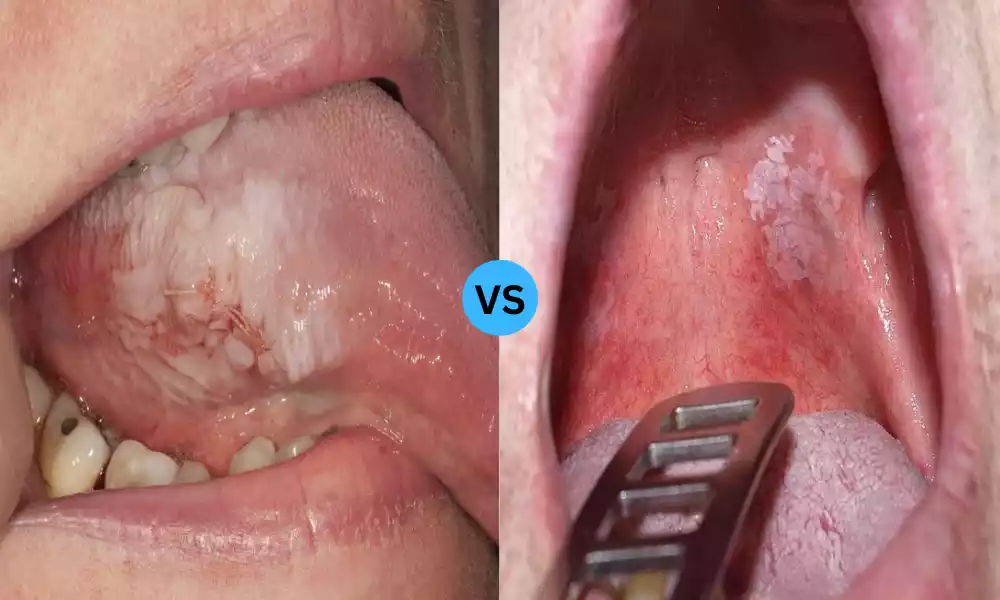
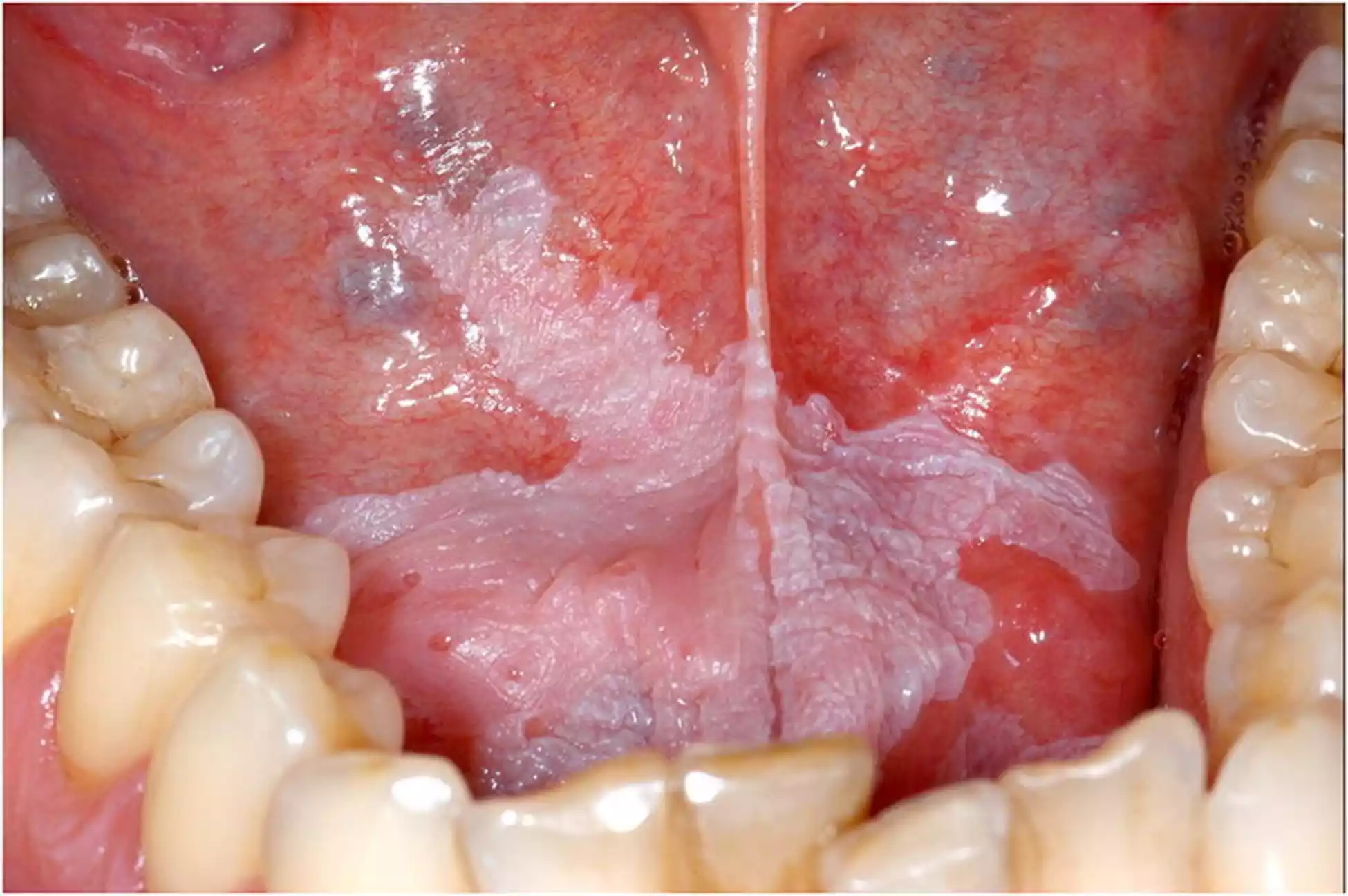
Tobacco Pouch Keratosis and Leukoplakia are two distinct oral conditions characterized by the presence of white lesions within the mouth. While they may appear similar at first glance, they have different causes and implications for an individual’s health. Tobacco Pouch Keratosis is primarily associated with the use of smokeless tobacco products and is not pre-cancerous, whereas Leukoplakia encompasses various white oral lesions and is potentially pre-cancerous. Understanding the differences between these conditions is crucial for accurate diagnosis, tailored treatment, and preventive measures, ultimately promoting better oral health and reducing the risk of oral cancer.
Definition of Tobacco Pouch Keratosis
Tobacco Pouch Keratosis, also known as Snuff Dipper’s Lesion, is a condition that affects the oral mucosa, specifically in individuals who use smokeless tobacco products such as chewing tobacco, snuff, or snus. It is characterized by the presence of white, keratotic (thickened) lesions that develop in the area where the tobacco product is habitually placed in the mouth.

These lesions are generally localized and can range in size and appearance. Importantly, Tobacco Pouch Keratosis is not a pre-cancerous condition, but it is crucial to monitor these lesions due to the association between smokeless tobacco and oral cancer.
Causes
The causes of Tobacco Pouch Keratosis:
- Chronic Use of Smokeless Tobacco: The primary cause is the habitual use of smokeless tobacco products, including chewing tobacco, snuff, or snus.
- Nicotine Exposure: Smokeless tobacco products contain nicotine, which is a highly addictive substance and a key contributor to the development of keratotic lesions.
- Tobacco-Specific Nitrosamines: These carcinogenic compounds present in smokeless tobacco can irritate and damage the oral mucosa, leading to the formation of lesions.
- Other Additives: Various additives in smokeless tobacco products can further contribute to the chronic irritation and changes in oral tissues associated with Tobacco Pouch Keratosis.
Symptoms
The symptoms of Tobacco Pouch Keratosis are relatively straightforward. Individuals with this condition will typically exhibit the following signs:
- White Lesions: The hallmark sign is the presence of white, thickened lesions on the oral mucosa. These may vary in size and shape but are typically located in areas where the smokeless tobacco product is held, such as the buccal mucosa (cheek), gingiva (gums), or the vestibule (the space between the lips and gums).
- No Pain or Discomfort: Unlike some oral conditions, Tobacco Pouch Keratosis is typically painless and does not cause discomfort or burning sensations.
- Persistence: These lesions tend to be persistent and do not resolve on their own, even after the individual stops using smokeless tobacco.
- No Pre-cancerous Changes: It’s important to note that Tobacco Pouch Keratosis is distinct from pre-cancerous or cancerous lesions, and it does not transform into oral cancer itself.
Definition of Leukoplakia
Leukoplakia, on the other hand, is a clinical term used to describe white patches or plaques that develop on the mucous membranes of the oral cavity, as well as other areas of the body such as the genitalia. These patches may have a slightly raised, wrinkled appearance and cannot be characterized as being caused by any specific irritant, such as smokeless tobacco. Leukoplakia, in itself, is a clinical diagnosis and not a definitive pathological diagnosis; it serves as an umbrella term for white oral lesions that do not fit into another diagnostic category.
Causes
The primary cause of Leukoplakia is chronic irritation or trauma to the oral mucosa. Unlike Tobacco Pouch Keratosis, Leukoplakia is not directly linked to any specific substance. Several factors can contribute to the development of these lesions, including:
- Tobacco Use: While Leukoplakia is not limited to tobacco users, smoking and other forms of tobacco use can irritate the oral mucosa, increasing the risk of developing these white patches.
- Alcohol Consumption: Excessive alcohol consumption, especially when combined with tobacco use, can increase the risk of Leukoplakia.
- Chronic Irritation: Sharp teeth, dentures that do not fit properly, rough dental fillings, or other mechanical factors can cause chronic irritation and contribute to the formation of Leukoplakia.
- Viral Infections: Certain viral infections, such as the human papillomavirus (HPV), have been associated with some cases of Leukoplakia.
- Immunosuppression: Weakened immune systems, whether due to diseases like HIV or the use of immunosuppressive medications, can increase the risk of developing Leukoplakia.
- Unknown Causes: In some cases, the cause of Leukoplakia may be unknown, and it may develop without an obvious triggering factor.
Symptoms
The symptoms of Leukoplakia can vary depending on the location and severity of the lesions. Common signs and symptoms include:
- White Patches: As the primary characteristic, white patches or plaques are typically seen on the tongue, buccal mucosa, gingiva, or other areas within the oral cavity.
- Rough or Scaly Texture: The patches may have a rough or scaly texture and might appear raised or slightly elevated from the surrounding tissues.
- No Pain: Leukoplakia is often painless and does not cause discomfort or burning sensations in most cases.
- Persistence: Like Tobacco Pouch Keratosis, Leukoplakia lesions tend to be persistent and do not resolve spontaneously.
Leukoplakia is considered a potentially pre-cancerous condition. While not all cases of Leukoplakia will progress to cancer, it is a strong indication for close monitoring and appropriate management.
Importance of Distinguishing Between Tobacco Pouch Keratosis and Leukoplakia
Distinguishing between Tobacco Pouch Keratosis and Leukoplakia is of paramount importance for several key reasons:
- Treatment and Management: The management and treatment of these conditions differ significantly. While Tobacco Pouch Keratosis is not pre-cancerous and often requires only tobacco cessation and monitoring, Leukoplakia is a potentially pre-cancerous lesion that necessitates more aggressive monitoring, potential biopsies, and interventions to reduce the risk of malignant transformation.
- Oral Cancer Risk: Leukoplakia, being potentially pre-cancerous, has a more direct association with the development of oral cancer. Early identification and intervention can significantly reduce the risk of malignant transformation. In contrast, Tobacco Pouch Keratosis, while still requiring monitoring, is not inherently pre-cancerous, and the risk of oral cancer is lower.
- Risk Factors and Prevention: Distinguishing between these conditions helps guide prevention efforts. Individuals with Tobacco Pouch Keratosis need education about the risks of smokeless tobacco and the importance of quitting these products. Those with Leukoplakia must be aware of the risk factors associated with this condition and take measures to reduce them, such as quitting smoking and moderating alcohol consumption.
- Public Health Implications: Clear differentiation is crucial from a public health perspective. Tobacco use, in any form, remains a significant health concern. Public health initiatives that aim to reduce tobacco use, especially among the youth, can contribute to the prevention of both Tobacco Pouch Keratosis and Leukoplakia.
- Lifestyle and Behavioral Changes: Understanding the specific causes and risk factors for these conditions can inform lifestyle changes and behavioral interventions. By distinguishing between them, healthcare providers can provide more tailored advice and support to individuals at risk.
- Timely Intervention: Early diagnosis and proper identification of Leukoplakia can lead to timely interventions that can prevent or address pre-cancerous changes. This significantly improves the chances of successful outcomes and reduces the need for extensive treatments.
- Quality of Life: Early detection and intervention can help individuals maintain a higher quality of life by preventing the need for disfiguring surgeries and other complications associated with advanced oral cancer.
- Public Awareness: Differentiating between these conditions helps raise public awareness of the risks associated with tobacco and alcohol use, encouraging individuals to make informed decisions about their oral health.
Understanding the difference between Tobacco Pouch Keratosis and Leukoplakia is crucial for proper diagnosis, treatment, prevention, and public health efforts, ultimately contributing to improved oral health and reduced risks of oral cancer.
Comparison Table of Tobacco Pouch Keratosis and Leukoplakia
To provide a concise overview of the distinctions between Tobacco Pouch Keratosis and Leukoplakia, here is a comparison table:
| Aspect | Tobacco Pouch Keratosis | Leukoplakia |
| Etiology | Linked to smokeless tobacco use | Multiple potential causes |
| Appearance | Thick, localized white lesions | Variable appearance, often wrinkled |
| Malignant Potential | Not pre-cancerous | Potentially pre-cancerous |
| Management | Cessation of tobacco use | Multifaceted, addressing causes and monitoring |
| Histology | Hyperkeratosis, acanthosis | Variable may include pre-cancerous changes |
| Location | Specific to the site of tobacco use | Can occur in various oral regions |
Similarities Between Tobacco Pouch Keratosis and Leukoplakia
While Tobacco Pouch Keratosis and Leukoplakia are distinct oral conditions with notable differences, they also share some similarities, which include:
- White Lesions: Both conditions present as white lesions or patches within the oral cavity. These lesions may vary in appearance and texture, but their commonality is the presence of white areas on the oral mucosa.
- Persistence: The white lesions associated with both Tobacco Pouch Keratosis and Leukoplakia are generally persistent and do not resolve on their own. They tend to remain in place for an extended period, which underscores the importance of seeking professional evaluation.
- Lack of Pain: In most cases, neither condition is associated with pain or discomfort. Individuals with these lesions typically do not experience pain or burning sensations, making them relatively painless conditions.
- Importance of Monitoring: Regular monitoring is essential for both conditions. In the case of Tobacco Pouch Keratosis, monitoring is necessary to ensure that the lesions do not worsen or lead to other complications. For Leukoplakia, monitoring is critical due to its potential to progress to oral cancer or exhibit pre-cancerous changes.
- Association with Risk Factors: While the primary risk factor for Tobacco Pouch Keratosis is the use of smokeless tobacco products, both conditions are associated with certain risk factors. These shared risk factors include tobacco use (though in the case of Leukoplakia, this includes not only smokeless but also smoking), alcohol consumption, and, to some extent, viral infections.
These similarities underscore the importance of proper diagnosis and monitoring by a healthcare professional to differentiate between the two conditions and determine the appropriate course of action, whether it be tobacco cessation, addressing other risk factors, or more extensive interventions.
Diagnosis of Tobacco Pouch Keratosis and Leukoplakia
Diagnosing both Tobacco Pouch Keratosis and Leukoplakia involves a thorough clinical examination, often performed by a dentist or oral healthcare provider. Below is a breakdown of what constitutes a complete process:
- Clinical Examination:
- Visual Inspection: The healthcare provider will visually examine the oral cavity, looking for white lesions. They will note the location, appearance, and any other relevant characteristics.
- Tobacco Use History: For individuals with white oral lesions, a detailed history of tobacco use is crucial in differentiating between the two conditions. A history of smokeless tobacco use strongly suggests Tobacco Pouch Keratosis.
- Risk Factors: The healthcare provider will inquire about other risk factors such as alcohol consumption and any other relevant medical history.
- Biopsy:
- Leukoplakia: When Leukoplakia is suspected, a biopsy may be performed. During a biopsy, a small sample of the lesion is removed for pathological examination. This is a critical step to assess whether the lesion has pre-cancerous or cancerous changes.
- Tobacco Pouch Keratosis: Biopsy is generally not necessary for Tobacco Pouch Keratosis because the condition is primarily related to the use of smokeless tobacco and does not inherently carry pre-cancerous changes.
- Histological Examination:
- Histopathology: For Leukoplakia cases, the biopsy sample is sent to a pathology laboratory for histological examination. This examination will determine whether the lesion shows signs of pre-cancerous or cancerous changes.
- Additional Tests:
- HPV Testing: In some cases, particularly when the lesions are associated with the human papillomavirus (HPV), specific tests may be conducted to identify the viral infection.
The diagnosis is crucial in distinguishing between Tobacco Pouch Keratosis and Leukoplakia, as it guides subsequent management and treatment decisions.
Treatment Approaches
The management and treatment of Tobacco Pouch Keratosis and Leukoplakia differ significantly due to their distinct etiologies and potential for malignant transformation.
Treatment of Tobacco Pouch Keratosis:
The primary approach to managing Tobacco Pouch Keratosis involves the following steps:
- Cessation of Tobacco Use: The most critical step in managing Tobacco Pouch Keratosis is quitting the use of smokeless tobacco products. This is often challenging due to the addictive nature of tobacco, but it is essential to halt the progression of the condition.
- Regular Monitoring: Individuals with Tobacco Pouch Keratosis should have regular follow-up appointments with their oral healthcare provider. Monitoring is necessary to ensure that the lesions do not worsen or lead to complications.
- Education and Support: Healthcare providers can play a crucial role in educating and supporting individuals in their efforts to quit using tobacco. Smoking cessation programs, counseling, and nicotine replacement therapy may be recommended to aid in the process.
- Management of Complications: In rare cases, Tobacco Pouch Keratosis can lead to severe complications, such as the formation of ulcers or other lesions. These complications may require additional treatment, such as topical medications to promote healing.
Treatment of Leukoplakia:
The management of Leukoplakia is more comprehensive due to its pre-cancerous nature. It involves the following steps:
- Identification of Underlying Causes: The first step in managing Leukoplakia is identifying and addressing the underlying causes. This may include quitting smoking, reducing alcohol consumption, and addressing any other risk factors.
- Regular Monitoring: Like Tobacco Pouch Keratosis, individuals with Leukoplakia need regular follow-up appointments for clinical examination and monitoring.
- Biopsy and Histological Examination: If the clinical evaluation suggests pre-cancerous or cancerous changes, a biopsy is performed to confirm the diagnosis. The histological examination guides further management.
- Interventions: Depending on the histological findings and the clinical course, interventions may be necessary. These interventions can range from surgical excision of the lesion to more extensive treatments like laser therapy or cryotherapy.
- Continued Risk Reduction: Even after treatment, individuals with a history of Leukoplakia must continue to reduce risk factors, such as abstaining from tobacco and limiting alcohol consumption. This is critical to prevent recurrence and further complications.
- Supportive Care: In cases where interventions are performed, individuals may require supportive care to manage pain, discomfort, and promote healing.
The Importance of Early Detection
The importance of early detection cannot be overstated when it comes to both Tobacco Pouch Keratosis and Leukoplakia.

Here are the key reasons for early detection:
- Prevention of Oral Cancer:
For Leukoplakia, early detection and intervention are crucial for preventing the progression of oral cancer. Timely identification of pre-cancerous or cancerous changes allows for early treatment, which greatly improves the chances of a successful outcome.
- Risk Reduction:
Early detection provides an opportunity to address risk factors associated with both conditions. In the case of Leukoplakia, identifying and addressing the underlying causes (e.g., tobacco and alcohol use) can significantly reduce the risk of malignant transformation. For Tobacco Pouch Keratosis, quitting smokeless tobacco reduces the risk of oral cancer.
- Better Outcomes:
Treatment outcomes are generally more favorable when conditions are detected in their early stages. The management of both Tobacco Pouch Keratosis and Leukoplakia is more effective when initiated promptly.
- Improved Quality of Life:
Early detection and treatment can help individuals maintain a higher quality of life by preventing the need for more aggressive interventions and potentially disfiguring surgeries associated with advanced oral cancer.
- Public Health Impact:
Early detection can contribute to public health efforts to reduce the burden of oral cancer and other associated health issues. Identifying cases early allows for targeted interventions and educational programs.
Lifestyle Changes and Prevention
Preventing both Tobacco Pouch Keratosis and Leukoplakia primarily revolves around making lifestyle changes and reducing risk factors. Here are key steps to consider:
- Tobacco Cessation:
- Tobacco Pouch Keratosis: Quitting the use of smokeless tobacco products is the most effective way to prevent this condition. Seek support from healthcare providers, smoking cessation programs, or support groups to overcome addiction.
- Leukoplakia: For Leukoplakia, quitting all forms of tobacco use is essential to reduce the risk of malignant transformation.
- Alcohol Moderation:
- Leukoplakia: Reducing alcohol consumption, especially when combined with tobacco use, can help lower the risk of developing Leukoplakia.
- Good Oral Hygiene:
- Maintaining good oral hygiene practices, including regular brushing and flossing, can contribute to oral health and reduce the risk of chronic irritation that may lead to these conditions.
- Regular Dental Checkups:
- Scheduling regular dental checkups allows for the early detection of any oral changes, lesions, or risk factors that may contribute to the development of these conditions.
- Protection from Trauma:
- Avoiding habits that cause trauma to the oral mucosa, such as chewing on hard objects or using sharp dental instruments, can help prevent Leukoplakia.
- HPV Vaccination:
- Reducing the risk of oral HPV infection may help prevent some cases of Leukoplakia. HPV vaccines are recommended and available to younger individuals.
- Education and Awareness:
- Public health initiatives aimed at educating individuals about the risks associated with tobacco use, excessive alcohol consumption, and other risk factors can contribute to prevention efforts.
Summary
Tobacco Pouch Keratosis and Leukoplakia, both presenting as white oral lesions, differ significantly in causes and potential consequences. While Tobacco Pouch Keratosis results from smokeless tobacco use and is not pre-cancerous, Leukoplakia can have various causes and carries a potential risk of malignancy. Distinguishing between them is crucial for tailored treatment, early cancer prevention, and risk factor management.
Public awareness and lifestyle changes, including tobacco cessation and moderation of alcohol consumption, play a vital role in reducing the prevalence of these conditions and associated oral cancer risks. Regular monitoring and timely intervention are key to ensuring better oral health outcomes.